10 Best Anti Inflammatory Supplements 2025: Reversing the Hidden Cause of Aging and Chronic Disease
The immense majority of diseases have one common denominator: Inflammation. Considering how functional foods and nutraceuticals have inflammation-reducing benefits, these products can have an extensive range of applications.
Inflammation is the body’s response to harmful stimulus such as injury,
infection, or irritation. There are two main types of inflammation ; acute
inflammation and chronic inflammation.
Chronic inflammation is a slower and milder form of inflammation that usually persists for more than six weeks. Unlike acute inflammation, which occurs in response to an injury or illness, chronic inflammation can occur without any apparent cause and can continue even after the underlying cause has been resolved. It has been linked to several conditions such as autoimmune disorders and prolonged stress.
The early part of the 21st century brought enormous
attention to the importance and value of vitamin D,
particularly in the treatment of autoimmune diseases like
Rheumatoid Arthritis.
Make sure to take 500 mg to 1000 mg of magnesium and 150 mcg of vitamin K2, (not K1) which are important cofactors for optimizing vitamin D function. And, remember the only way you know what your vitamin D level is, is to test it. Vitamin D level should be in a therapeutic range of 50 to 70 ng/ml for treatment of rheumatoid arthritis. Most people are shocked how low their level is when they finally get around to testing it.
With thousands of studies performed, researchers have shown curcumin has antibacterial, anticancer, anti-inflammatory, antimalarial, antioxidant, antiparasitic, antiproliferative, pro-apoptotic and wound healing properties.
It’s also available as a supplement. PubMed has indexed more than 3,900 research studies on curcumin and anti-inflammatory. However, most of the studies are non-human or pre-clinical studies.
Twenty-nine (29) RCTs involving 2396 participants and 5 types of arthritis were included.
A study published in a 2017 edition of the journal Foods confirmed that curcumin in turmeric has anti-inflammatory and antioxidant effects.
In 2019, some researchers found that curcumin capsules had a similar effect on the symptoms of knee osteoarthritis as diclofenac, an NSAID.
In the study, 139 people with OsteoArthritis of the knee took either a 50-milligram tablet of diclofenac twice a day for 28 days or a 500-milligram curcumin capsule three times a day.
Both groups said their pain levels improved, but those who took curcumin had fewer negative effects. The research suggested that people who can’t take NSAIDs may be able to use curcumin instead.
While turmeric is widely available in powdered form, it contains a very small amount of curcumin, which is also known to be poorly absorbed through your gastrointestinal tract. For these reasons, you’ll receive more health benefits from a curcumin extract. Because it's a lipophilic (fat-loving) molecule, many curcumin preparations include some sort of oil or fat to improve its absorbability and bioavailability.
Existing meta-analyses on omega-3 polyunsaturated fatty acids and their anti-inflammatory effects have reported uncertain findings. The umbrella meta-analysis (published in 2022) aimed to assess the findings of multiple meta-analyses on the efficacy of omega-3 fatty acids on inflammatory biomarkers in adults with different health conditions.
Research suggests glucosamine and chondroitin work synergistically when paired, and MSM can further boost their effects by enhancing cell penetration. All three have anti-inflammatory properties and are commonly used in the treatment of arthritis symptoms.
Many clinical studies have found that chondroitin can reduce
joint pain and stiffness in people with osteoarthritis. PubMed
has indexed more than 700 research studies on glucosamine and anti-inflammatory. Joint supplements often combine glucosamine with
chondroitin.
Sally Norton, author of “Toxic Superfoods: How Oxalate Overload Is Making You Sick — and How to Get Better,” explains:
For these reasons, if you take vitamin C on a regular basis, Norton recommends limiting it to 250 mg a day. This is enough to meet your nutritional requirements and is unlikely to cause oxalic acid-related trouble. The exception would be if you are septic, in which case large doses of IV ascorbic acid can save your life.
Related:
How Vitamin C Is Effective in Treating Inflammatory Issues
In a 2020 randomized controlled trial, mineral rich algae with pine bark improved pain,
physical function and analgesic use in mild-knee joint
osteoarthritis, compared to Glucosamine.
Related:
Pycnogenol vs Pine Bark Extract
Vitamin E can almost miraculously prevent most of the damage done by LA, and it can also reverse or prevent many of the issues associated with excess estrogen. This is important because LA has remarkable parallels to excess estrogen in terms of its metabolic and anti-health effects. You see, when you eat excess PUFA or LA, you increase your body's production of estrogen.
So, when you increase LA, estrogen levels go up — and that's not a good thing. Both LA and estrogen interestingly increase the flow of calcium from outside the cell to inside because the concentration of calcium outside as well is 50 times higher than inside. So, the excess as LA will cause the influx of calcium inside the cell, which causes nitric oxide and superoxide to increase inside the cell.
When you do this, with this magical combination, you increase a very pernicious reactive nitrogen species called peroxynitrite, and that causes pervasive damage to tissues in your body.
Both LA and estrogen also increase a potentially dangerous process in your body called lipolysis, which is simply the liberation of fatty acids from your fat cells into your bloodstream where they are mobilized. This then increases the oxidation or, simply, the burning of fats in your mitochondria, which is precisely what you want to avoid as ideally you want to be burning glucose in your mitochondria, not fatty acids.
Fortunately, vitamin E can help neutralize this damaging effect of LA. Vitamin E also directly inhibits the activity of an enzyme called aromatase. This is an enzyme that converts the male hormones like testosterone and DHEA into estrogens.
Even better, it serves as an estrogen antagonist, meaning it binds to the estrogen receptor to block it from binding to estrogen. This dramatically lowers the damage from excess estrogen.
Vitamin E works very similarly to the drug tamoxifen, which is used to treat estrogen receptor-positive breast cancers. For these reasons, I firmly believe nearly everyone needs to be getting vitamin E in their diet. However, due to the high LA burden, very few people are able to get enough vitamin E from their diet to suppress this oxidative destruction from excess LA in their tissues.
The good news is that since the supplementation is short term, you're not going to need it the rest of your life.
If you can keep your LA intake to below 5 grams a day for three years, it's likely you may not even need it at all, or at most, only a few times a month. However, if for whatever reason, during this time, or when the LA in your tissues are low or normal, and you go out and binge on a meal that's very high in LA, I would strongly recommend taking a vitamin E capsule to protect yourself from this exposure.
Vitamin E also protects against free radical damage and the normal effects of aging. It’s particularly important for brain health, and studies have found it can help delay the loss of cognitive function in people with Alzheimer’s disease by preventing cell membrane damage and neuronal death.1
How to Pick a Good Vitamin E Supplement

Chronic, low-grade inflammation is a
hallmark of aging
associated with numerous age-related diseases. Interestingly,
magnesium plays a significant role in modulating your body's
inflammatory responses. When your magnesium levels are low, your
body produces more inflammatory cytokines like IL-1, IL-6 and
TNF-α. These inflammatory markers are linked to various chronic
conditions, including cardiovascular disease and diabetes.
On the flip side, adequate magnesium levels help suppress the production of these inflammatory substances. Magnesium also helps activate your body's antioxidant defense systems, protecting your cells from oxidative stress and further reducing inflammation. Studies have shown that people with higher magnesium intake have lower levels of C-reactive protein, a key marker of inflammation. (Nutrients 2024)
By ensuring you're getting enough magnesium, you're not just supporting your energy production — you're also giving your body a powerful tool to combat chronic inflammation and reduce your risk of age-related diseases.
In one human study, 20 patients with rheumatoid arthritis drank 0.5 L/day of hydrogen water for 4 weeks. By the end of the study, all patients with early rheumatoid arthritis achieved remission and
20% became symptom-free [R].
Related: FENBENDAZOLE Testimonials in Multiple Sclerosis, Rheumatoid Arthritis and Osteoarthritis.
In summary, when combined with an anti-inflammatory diet, proper vitamin and mineral supplementation can be a true game-changer when it comes to fighting chronic inflammation. But, instead of going and buying every single supplement mentioned in this article, we encourage you to connect with a trusted functional medical practitioner to help you map out the best approach for your unique goals and health history.
Keep in mind that the best anti-inflammatory supplements will never mask poor sleep habits and a highly-processed diet.
Acute inflammation usually restores your body to its state before injury or
illness. It often resolves in two weeks or less. Symptoms appear quickly.
Chronic inflammation is a slower and milder form of inflammation that usually persists for more than six weeks. Unlike acute inflammation, which occurs in response to an injury or illness, chronic inflammation can occur without any apparent cause and can continue even after the underlying cause has been resolved. It has been linked to several conditions such as autoimmune disorders and prolonged stress.
A
study published in Nature Medicine (2019) summarizes the causes of chronic inflammation and its
consequences. Some of the most common factors are physical inactivity,
obesity, a poor diet, social isolation, psychological stress, and poor
sleep.
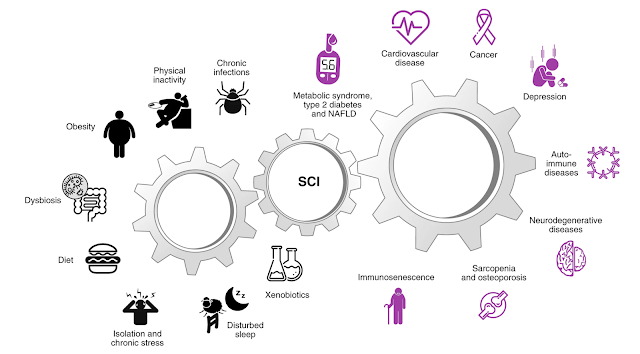
|
| Causes and consequences of low-grade systemic chronic inflammation (Nature Medicine) |
Best Anti Inflammatory Supplements
What are the most powerful and popular anti inflammatory
supplements? We researched the literature, and scoured the
internet to determine the best supplements for inflammation.
1. Vitamin D3 and K2
Perhaps bone health and sunlight is what comes to your mind when you hear “Vitamin D” but very few of us realize vitamin D’s capacity to manage inflammation. PubMed has indexed more than 1,700 research studies on vitamin D and anti-inflammatory.
The production of inflammatory proteins (cytokines) and
immune cells is better regulated when Vitamin D levels are
optimized. This is crucial for preventing the development
of many immune-related diseases (R).
In fact, one 2012 study showed that individuals with adequate vitamin D levels did not experience the typical inflammatory cascade. Those with subpar vitamin D levels failed to inhibit the inflammatory cascade (R).
In fact, one 2012 study showed that individuals with adequate vitamin D levels did not experience the typical inflammatory cascade. Those with subpar vitamin D levels failed to inhibit the inflammatory cascade (R).
Vitamin D3, also known as cholecalciferol, is the best
form of vitamin D. D3 is the natural form of vitamin D. It
is what our body makes when we are exposed to
sunlight.
Eating egg yolks might allow for sufficient vitamin D levels. Be sure to take your D3 with a meal as vitamin D is a fat-soluble vitamin.
Eating egg yolks might allow for sufficient vitamin D levels. Be sure to take your D3 with a meal as vitamin D is a fat-soluble vitamin.
Make sure to take 500 mg to 1000 mg of magnesium and 150 mcg of vitamin K2, (not K1) which are important cofactors for optimizing vitamin D function. And, remember the only way you know what your vitamin D level is, is to test it. Vitamin D level should be in a therapeutic range of 50 to 70 ng/ml for treatment of rheumatoid arthritis. Most people are shocked how low their level is when they finally get around to testing it.
Vitamin D and Omega-3 Lower Autoimmune Disease Risk
Researchers from Brigham and Women’s Hospital, Harvard Medical School, used data from the vitamin D and omega-3 trial (VITAL), which involved 25,871 participants aged 50 (men) or 55 (women) and older, to investigate whether vitamin D and omega-3 fats from marine sources reduce the risk of autoimmune disease. (BMJ 2022)
Participants took vitamin D3 (2,000 IU), omega-3 fats (1,000 milligrams) or a placebo daily and were followed for more than five years. They self-reported all autoimmune diseases that were diagnosed during the study period, and those taking vitamin D and/or omega-3s had a lower risk.
“Vitamin D supplementation for five years, with or without omega-3 fatty acids, reduced autoimmune disease by 22%, while omega-3 fatty acid supplementation with or without vitamin D reduced the autoimmune disease rate by 15% (not statistically significant),” the researchers wrote.
For those taking both vitamin D and omega-3 fats, the risk of autoimmune disease decreased by about 30%.6 Further, when participants took vitamin D for at least two years, their risk of autoimmune disease decreased even more — by 39%.
Vitamin D’s involvement in inflammation and both acquired and innate immune responses may explain why it appears to beneficial for preventing autoimmune diseases. Vitamin D receptors are present in nearly all cells of the human immune system, including monocytes/macrophages, T cells, B cells, natural killer cells and dendritic cells.
Participants took vitamin D3 (2,000 IU), omega-3 fats (1,000 milligrams) or a placebo daily and were followed for more than five years. They self-reported all autoimmune diseases that were diagnosed during the study period, and those taking vitamin D and/or omega-3s had a lower risk.
“Vitamin D supplementation for five years, with or without omega-3 fatty acids, reduced autoimmune disease by 22%, while omega-3 fatty acid supplementation with or without vitamin D reduced the autoimmune disease rate by 15% (not statistically significant),” the researchers wrote.
For those taking both vitamin D and omega-3 fats, the risk of autoimmune disease decreased by about 30%.6 Further, when participants took vitamin D for at least two years, their risk of autoimmune disease decreased even more — by 39%.
Vitamin D’s involvement in inflammation and both acquired and innate immune responses may explain why it appears to beneficial for preventing autoimmune diseases. Vitamin D receptors are present in nearly all cells of the human immune system, including monocytes/macrophages, T cells, B cells, natural killer cells and dendritic cells.
2. Turmeric (Curcumin) and Piperine (Black Pepper)
Curcumin is an antioxidant that may offer a variety of anti-inflammatory benefits. It’s present in turmeric, a mild spice that can add color and flavor to sweet and savory dishes, as well as teas.
It’s also available as a supplement. PubMed has indexed more than 3,900 research studies on curcumin and anti-inflammatory. However, most of the studies are non-human or pre-clinical studies.
In a systematic review and meta-analysis (published in 2023), major databases (PubMed, Scopus, Web of Science, Cochrane Library and Google Scholar) were searched from inception up to October 2022.
Main outcomes included inflammatory markers (i.e. C-reactive protein(CRP), tumour necrosis factorα(TNF-α), interleukin-6(IL-6), and interleukin 1 beta(IL-1β)) and markers of oxidative stress (i.e. total antioxidant capacity (TAC), malondialdehyde (MDA), and superoxide dismutase (SOD) activity).
Sixty-six RCTs (randomised controlled trials) were included in the final analysis. Authors observed that turmeric/curcumin supplementation significantly reduces levels of inflammatory markers, including CRP, TNF-α and IL-6 except for IL-1β for which no significant change was found. Also, turmeric/curcumin supplementation significantly improved anti-oxidant activity through enhancing TAC, reducing MDA levels, and SOD activity. It seems that turmeric/curcumin supplementation might be used as a viable intervention for improving inflammatory/oxidative status of individuals.
It is somewhat unbelievable how many articles have been published regarding turmeric’s ability to tackle inflammation in the human body. There is data to support just about every condition; Joint pain, digestion, Crohn’s Disease, heart disease, depression, cancer, cognition and eczema to name a few.
A 2022 meta-analysis of 29 RCTs (randomised controlled trials) concluded that curcumin may improve symptoms and inflammation levels in people with arthritis.
The arthritis included Ankylosing Spondylitis (AS), Rheumatoid Arthritis (RA), Osteoarthritis (OA), Juvenile idiopathic arthritis (JIA) and gout/hyperuricemia.
Curcumin and Curcuma longa Extract were administered in doses ranging from 120 mg to 1500 mg for a duration of 4-36 weeks. In general, Curcumin and Curcuma longa Extract showed safety in all studies and improved the severity of inflammation and pain levels in these arthritis patients.
Another 2021 meta-analysis on curcumin by researchers at the University of Miami, after reviewing 10 different studies on curcumin and knee arthritis with almost thirteen hundred patients, the researchers concluded that:
“Although limitations exist within the 10 RCTs reviewed, this small set of studies show a reduction in pain and improvement in function similar to that of NSAIDs but with a reduced incidence of adverse events. Turmeric appears to be a safe adjunct to NSAID therapy allowing for additional analgesic benefit as well as a reduced dosage requirement for NSAIDs. “
A study published in a 2017 edition of the journal Foods confirmed that curcumin in turmeric has anti-inflammatory and antioxidant effects.
In 2019, some researchers found that curcumin capsules had a similar effect on the symptoms of knee osteoarthritis as diclofenac, an NSAID.
In the study, 139 people with OsteoArthritis of the knee took either a 50-milligram tablet of diclofenac twice a day for 28 days or a 500-milligram curcumin capsule three times a day.
Both groups said their pain levels improved, but those who took curcumin had fewer negative effects. The research suggested that people who can’t take NSAIDs may be able to use curcumin instead.
Curcumin and Piperine / Black Pepper
Piperine is a natural substance that enhances the absorption of curcumin by 2,000% (Source). Curcumin supplements with piperine are substantially more effective compared to plain curcumin supplements.
The anti-inflammatory properties of both turmeric and piperine may aid in reducing gut inflammation, which can help with digestion. When combined, curcumin and piperine tend to have a greater effect on inflammation, digestion, reducing pain and fighting cancer.
Where to buy bioavailable curcumin: Ultra Botanica’s LPS technology UltraCur (UltraCurcumin)
3. Omega-3 Fish Oil
Omega-3 fatty acids are essential fats, meaning you must get them from the food you eat, as your body can’t make them. PubMed has indexed more than 2,000 research studies on omega-3 and anti-inflammatory.Note: A single meta-analysis of a treatment comparison for a single outcome offers a limited view if there are many treatments or many important outcomes to consider. Umbrella reviews assemble together several systematic reviews on the same condition.
Overall, 32 meta-analyses were qualified in this umbrella meta-analysis. The findings demonstrated that the omega-3 fatty acids supplementation significantly reduced serum C-reactive protein (CRP), Tumour necrosis factor α (TNFα), and interleukin 6 (IL-6) concentrations.
The umbrella meta-analysis (Kavyani 2022) found that supplementation of omega-3 in adults can improve CRP, TNF-α, and IL-6 concentrations under various health conditions. Omega-3 can be recommended as adjuvant anti-inflammatory agents.
Omega-3 fatty acids have also been associated with numerous health benefits, such as a reduced risk of heart disease, reduced inflammation, and improved mood (Source, Source, Source).
Fish oil and flaxseed oil each contain an impressive amount of omega-3 fatty acids.
The main types of omega-3s in fish oil are eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) (Source).
On the other hand, flaxseed oil contains the omega-3 fatty acid known as alpha-linoleic acid (ALA) (Source). Flaxseed oil also contains linoleic acid, an omega-6 fatty acid.
EPA and DHA are predominantly found in animal foods like fatty fish, while ALA is mostly found in plants.
However, ALA isn’t biologically active and needs to be converted to EPA and DHA to be used for something other than just stored energy like other types of fat (Source).
While ALA is still an essential fatty acid, EPA and DHA are linked to many more health benefits (Source). Additionally, the conversion process from ALA to EPA and DHA is quite inefficient in humans (Source). For example, one study found that only 5% of ALA is converted to EPA and less than 0.5% of ALA is converted to DHA in adults (Source).
EPA and DHA can reduce inflammation, which causes swelling and pain. Research has indicated that both acids might suppress the body’s immune system. However, a 2016 study suggests that DHA might enhance immune function instead. DHA is more effective at reducing inflammation than EPA, but both have a role.
All of these effects makes fish oil potentially beneficial for people with arthritis.
EPA and DHA come with other health benefits: They can help prevent heart attacks by making it harder for blood to clot. They help lower blood triglyceride levels and blood pressure. As well, EPA taken with statin medication is more effective in reducing the inflammation of arteriosclerosis than medication alone.
For the omega-3 fatty acids in fish oil to work against arthritis, it’s necessary to consume a fairly large quantity of it each day. Fish oil — or cod liver oil — enclosed in capsules makes this fairly easy.
On the other hand, because cod liver oil contains very high amounts of vitamin A and vitamin D, taking too much can be toxic. For the purpose of treating arthritis, fish oil is the safer choice.
*TOTOX value stands for total oxidation value. The omega 3 fatty acids EPA and DHA from fish oil are highly sensitive to oxidation. This means that they are rapidly affected by contact with oxygen. Oxidised fatty acids are not beneficial to our health. For this reason, a good fish oil supplement has a low TOTOX value. The maximum TOTOX value is set at 26 by the Global Organization for EPA and DHA omega-3.
We recommend taking a maximum of 1 gram of omega-3 per day. Higher amounts could be risky, because EPA and DHA are both polyunsaturated fats (PUFAs) and, like linoleic acid (LA), are susceptible to oxidation and the production of dangerous aldehyde metabolites.
Omega-3 fatty acids have also been associated with numerous health benefits, such as a reduced risk of heart disease, reduced inflammation, and improved mood (Source, Source, Source).
Fish oil and flaxseed oil each contain an impressive amount of omega-3 fatty acids.
The main types of omega-3s in fish oil are eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) (Source).
On the other hand, flaxseed oil contains the omega-3 fatty acid known as alpha-linoleic acid (ALA) (Source). Flaxseed oil also contains linoleic acid, an omega-6 fatty acid.
EPA and DHA are predominantly found in animal foods like fatty fish, while ALA is mostly found in plants.
However, ALA isn’t biologically active and needs to be converted to EPA and DHA to be used for something other than just stored energy like other types of fat (Source).
While ALA is still an essential fatty acid, EPA and DHA are linked to many more health benefits (Source). Additionally, the conversion process from ALA to EPA and DHA is quite inefficient in humans (Source). For example, one study found that only 5% of ALA is converted to EPA and less than 0.5% of ALA is converted to DHA in adults (Source).
EPA and DHA can reduce inflammation, which causes swelling and pain. Research has indicated that both acids might suppress the body’s immune system. However, a 2016 study suggests that DHA might enhance immune function instead. DHA is more effective at reducing inflammation than EPA, but both have a role.
All of these effects makes fish oil potentially beneficial for people with arthritis.
EPA and DHA come with other health benefits: They can help prevent heart attacks by making it harder for blood to clot. They help lower blood triglyceride levels and blood pressure. As well, EPA taken with statin medication is more effective in reducing the inflammation of arteriosclerosis than medication alone.
For the omega-3 fatty acids in fish oil to work against arthritis, it’s necessary to consume a fairly large quantity of it each day. Fish oil — or cod liver oil — enclosed in capsules makes this fairly easy.
On the other hand, because cod liver oil contains very high amounts of vitamin A and vitamin D, taking too much can be toxic. For the purpose of treating arthritis, fish oil is the safer choice.
According to a review (Nutrients, September 2022), data from scientific literature 'overwhelmingly' supports beneficial effects of omega-3 fatty acids on the length of telomeres, reported to be a marker of biological age.
Many governments recommend eating omega-3 containing fatty fish, two times per week. But that is often not enough. Ideally, people would need to eat fatty fish four times per week, while also supplementing with omega-3 fatty acids, at least 1,000 mg of pure omega-3 (DHA and EPA) per day.
Make sure you buy high-quality omega-3 fatty acid supplements, meaning that the omega-3 fatty acids are pure and have not oxidized much (having low “TOTOX” value*).
Many governments recommend eating omega-3 containing fatty fish, two times per week. But that is often not enough. Ideally, people would need to eat fatty fish four times per week, while also supplementing with omega-3 fatty acids, at least 1,000 mg of pure omega-3 (DHA and EPA) per day.
Make sure you buy high-quality omega-3 fatty acid supplements, meaning that the omega-3 fatty acids are pure and have not oxidized much (having low “TOTOX” value*).
Shop for fish oil supplement.
Omega-3 Dosage
4. Chondroitin, Glucosamine and MSM
Glucosamine and chondroitin are compounds found in human cartilage, while MSM (methylsulfonylmethane) is a sulphur-rich compound found in certain plants, fruits and vegetables.Research suggests glucosamine and chondroitin work synergistically when paired, and MSM can further boost their effects by enhancing cell penetration. All three have anti-inflammatory properties and are commonly used in the treatment of arthritis symptoms.
About 53 percent of people who take chondroitin have a 20 percent or
greater improvement in knee pain.
Chondroitin sulfate may also slow down the progression of osteoarthritis when taken long-term. Studies show that it slows down narrowing of the joint space when taken for up to 2 years.
In a 2022 meta-analysis of 8 randomized controlled trials, that included more than 3,700 patients; confirmed that the combination of glucosamine and chondroitin is effective and superior to other treatments in knee osteoarthritis to a certain extent.
Try it: Chondroitin is typically taken in a dose of 400 to 800 mg two or three times per day.
Chondroitin sulfate may also slow down the progression of osteoarthritis when taken long-term. Studies show that it slows down narrowing of the joint space when taken for up to 2 years.
In a 2022 meta-analysis of 8 randomized controlled trials, that included more than 3,700 patients; confirmed that the combination of glucosamine and chondroitin is effective and superior to other treatments in knee osteoarthritis to a certain extent.
Try it: Chondroitin is typically taken in a dose of 400 to 800 mg two or three times per day.
Methylsulfonylmethane (MSM)
Methylsulfonylmethane (MSM) is another common ingredient in
supplements said to help with joint pain. PubMed has indexed
more than 70 research studies on methylsulfonylmethane and anti-inflammatory.
One of the most popular uses of MSM is to decrease joint or
muscle pain. It has been shown to benefit those with joint
degeneration, a common cause of pain in the knees, back,
hands and hips.
A study in 100 people over the age of 50 found that treatment with a supplement containing 1,200 mg of MSM for 12 weeks decreased pain, stiffness and swelling in the joints, compared to a placebo (Int J Biomed Sci. 2015).
The group receiving the supplement also reported improved overall quality of life and less difficulty walking and getting out of bed (Int J Biomed Sci. 2015).
A study in 100 people over the age of 50 found that treatment with a supplement containing 1,200 mg of MSM for 12 weeks decreased pain, stiffness and swelling in the joints, compared to a placebo (Int J Biomed Sci. 2015).
The group receiving the supplement also reported improved overall quality of life and less difficulty walking and getting out of bed (Int J Biomed Sci. 2015).
In one randomised controlled study (2011), MSM improved pain and functioning compared to
a placebo in people with osteoarthritis.
Another study in 32 people with lower back pain found that taking a glucosamine supplement containing MSM significantly reduced lumbar stiffness and pain upon movement, plus greatly increased quality of life (Curr Ther Res Clin Exp. 2005).
Try it: Typical MSM doses range from 1,500 to 6,000 grams per day, sometimes divided into two doses.
Another study in 32 people with lower back pain found that taking a glucosamine supplement containing MSM significantly reduced lumbar stiffness and pain upon movement, plus greatly increased quality of life (Curr Ther Res Clin Exp. 2005).
Try it: Typical MSM doses range from 1,500 to 6,000 grams per day, sometimes divided into two doses.
5. Resveratrol, Quercetin, Pterostilbene and Bromelain
Resveratrol is another nutrient that has antioxidant and
anti-inflammatory properties. PubMed has indexed more than 2,000
research studies on resveratrol and anti-inflammatory.
In a 2018 study, scientists gave 110 people with mild to moderate OA of the
knee a 500-milligram dose of resveratrol or a placebo. They took
this combination alongside a 15-gram dose of the NSAID meloxicam
every day for 90 days.
People who took resveratrol found that their pain levels dropped significantly, compared with those who took the placebo. More research is needed to confirm that resveratrol can benefit people with OA.
However, if you’re already taking another NSAID and it doesn’t reduce your pain as much as you’d like, the research suggests Resveratrol may be a useful add-on.
People who took resveratrol found that their pain levels dropped significantly, compared with those who took the placebo. More research is needed to confirm that resveratrol can benefit people with OA.
However, if you’re already taking another NSAID and it doesn’t reduce your pain as much as you’d like, the research suggests Resveratrol may be a useful add-on.
Quercetin has also been shown to reduce inflammation in multiple
studies. In this 8 week study (2017) involving 50 women with rheumatoid arthritis,
participants took 500mg of quercetin per day or a placebo. The
quercetin group reported less early morning stiffness, morning
pain, and after-activity pain.
Early studies on quercetin and inflammation are promising, although more large scale human studies need to be performed to verify these benefits.
Early studies on quercetin and inflammation are promising, although more large scale human studies need to be performed to verify these benefits.
Most quercetin supplements contain Bromelain, as some evidence suggests they boost absorption.
Bromelain is an enzyme found in pineapples. It can also reduce
inflammation, joint pain and joint degradation, improve gut
function and digestive health, and aid in the metabolism of
amino acids. There’s also evidence suggesting it can help to
prevent respiratory issues and heart disease, and bolster immune
function. (R)
6. Vitamin C
Boosting your vitamin C intake also affects the inflammatory response in the body. PubMed has indexed more than 600 research studies on vitamin C and anti-inflammatory.
Vitamin C is a crucial component of a treatment protocol developed
by Dr. Paul Marik, previously a critical care doctor at Sentara
Norfolk General Hospital in East Virginia. The treatment protocol
was developed for sepsis, which is a life-threatening condition
triggered by a systemic infection that causes your body to
overreact and launch an excessive and damaging immune response.
According to a 2011 paper, the coagulation system, which is dysfunctional in sepsis, is closely related to the inflammatory response. The communication between the two systems drives the dysregulated response that ultimately results in a very high mortality rate.
According to a 2011 paper, the coagulation system, which is dysfunctional in sepsis, is closely related to the inflammatory response. The communication between the two systems drives the dysregulated response that ultimately results in a very high mortality rate.
Unless sepsis is diagnosed promptly and treated appropriately, it
can progress rapidly to multiple organ failure and death. This
includes cases of suspected
influenza since sepsis can mimic many of the signs and symptoms of
flu. Although severe sepsis has traditionally been linked to
bacterial infections, doctors are seeing more patients with severe
sepsis that are caused directly by influenza viruses.
Marik’s retrospective before-after clinical study showed giving patients 200 mg of thiamine every 12 hours, 1,500 mg of ascorbic acid every six hours, and 50 mg of hydrocortisone every six hours for two days reduced mortality from 40.4% to 8.5%.
As importantly, the treatment has no side effects and is inexpensive, readily available and simple to administer. In other words, there's virtually no risk involved. Research published in 2020 found Marik’s sepsis protocol lowered mortality in pediatric patients as well.
Utilizing vitamin C in the treatment of sepsis may help lower both mortality rate and cost. Each year an estimated 1.7 million Americans get sepsis, and nearly 270,000 of them die.
Conventional treatment focuses on high-dose antibiotics. A U.S. government report published in 2016 noted that sepsis was the most expensive condition treated in the U.S., racking up $23.7 billion in health care costs each year. By 2022, that had skyrocketed to $62 billion just for treatment and care.
Marik’s retrospective before-after clinical study showed giving patients 200 mg of thiamine every 12 hours, 1,500 mg of ascorbic acid every six hours, and 50 mg of hydrocortisone every six hours for two days reduced mortality from 40.4% to 8.5%.
As importantly, the treatment has no side effects and is inexpensive, readily available and simple to administer. In other words, there's virtually no risk involved. Research published in 2020 found Marik’s sepsis protocol lowered mortality in pediatric patients as well.
Utilizing vitamin C in the treatment of sepsis may help lower both mortality rate and cost. Each year an estimated 1.7 million Americans get sepsis, and nearly 270,000 of them die.
Conventional treatment focuses on high-dose antibiotics. A U.S. government report published in 2016 noted that sepsis was the most expensive condition treated in the U.S., racking up $23.7 billion in health care costs each year. By 2022, that had skyrocketed to $62 billion just for treatment and care.
Note: Vitamin C is known as an antioxidant, but at high
concentrations, vitamin C has a pro-oxidant property (Transl Oncol. 2020).
The Hazards of Excessive Vitamin C
Vitamin C and ascorbic acid can lead to problems if your body is
already loaded with oxalates as it is metabolically reduced to
oxalic acid during breakdown.
Sally Norton, author of “Toxic Superfoods: How Oxalate Overload Is Making You Sick — and How to Get Better,” explains:
“The major source of internal oxalate is ascorbic acid or
vitamin C ... There are lots of case studies of train wrecks
from supplements, and lots of case studies about problems with
intravenous vitamin C. Let me tell you my personal story. I
had vitamin C chelation ... I didn't know I had an oxalate
problem ...
By the third time, I became harder and harder to stab for the IV needle because now my veins were ropier and rollier and would run away from the needle. That's fibrosis ... I only had IV vitamin C maybe 10 times. But the doctor and the nurse took no notice of this side effect of the treatment — that I was becoming more fibrotic and harder to puncture ...
It's hubris to say, ‘Oh, well, it's fine. All my patients are doing great on my vitamin C IVs when you're not open to seeing the side effects. One of the studies demonstrated that just with oral supplementation, for not all that long, once they stopped the vitamin C, the level of oxalate in the urine went way up.
So, while the body's being assaulted by too much vitamin C, it's busy sequestering the oxalate that's forming and holding onto it and protecting the kidneys from devastation, from excessive oxalate load. Once you stop producing or eating too much oxalate, this holding pattern can let go, and now you see much higher oxalate levels in the blood and the urine.”
By the third time, I became harder and harder to stab for the IV needle because now my veins were ropier and rollier and would run away from the needle. That's fibrosis ... I only had IV vitamin C maybe 10 times. But the doctor and the nurse took no notice of this side effect of the treatment — that I was becoming more fibrotic and harder to puncture ...
It's hubris to say, ‘Oh, well, it's fine. All my patients are doing great on my vitamin C IVs when you're not open to seeing the side effects. One of the studies demonstrated that just with oral supplementation, for not all that long, once they stopped the vitamin C, the level of oxalate in the urine went way up.
So, while the body's being assaulted by too much vitamin C, it's busy sequestering the oxalate that's forming and holding onto it and protecting the kidneys from devastation, from excessive oxalate load. Once you stop producing or eating too much oxalate, this holding pattern can let go, and now you see much higher oxalate levels in the blood and the urine.”
For these reasons, if you take vitamin C on a regular basis, Norton recommends limiting it to 250 mg a day. This is enough to meet your nutritional requirements and is unlikely to cause oxalic acid-related trouble. The exception would be if you are septic, in which case large doses of IV ascorbic acid can save your life.
7. Zinc
PubMed has indexed more than 1,600 research studies on zinc and anti-inflammatory.
In this review, published in the Journal of Trace Elements in Medicine and Biology (2014), zinc is also an antioxidant and
anti-inflammatory agent. Zinc supplementation studies in the
elderly have shown decreased incidence of infections,
decreased oxidative stress, and decreased generation of
inflammatory cytokines. Decreased incidences of blindness in
patients with AMD and increased atheroprotective effect have
been observed in the zinc supplemented elderly.
Note: Atheroprotective effect means to prevent plaque
within the blood vessels.
8. Pine Bark Extract (Pycnogenol)
This is a relatively new comer in this anti inflammatory
space. PubMed has indexed more than 70 research studies
on pygnogenol and anti-inflammatory.
Pine bark acts as a local anti-inflammatory in synovial fluid
(R) and three publications have shown it to improve KOA (knee
osteoarthritis) pain and stiffness, NSAID (non steroidal anti
inflammatory drug) use, physical and emotional well-being (R, R, R). Pine bark preparations have recently been “strongly
recommended” to the rheumatology community as early and
additive treatment for OA, likely based on the following
meta-analysis (R, R).
9. Vitamin E
Vitamin E prevents LA stored in your tissues from being oxidized into dangerous toxic byproducts. Since most people are walking around with LA stores that are 10 times higher than normal, and since excess LA is likely one of the primary contributors to chronic disease, it can be a good idea to take vitamin E regularly until you get your LA down to healthy levels, which may take up to six years for most people.Vitamin E can almost miraculously prevent most of the damage done by LA, and it can also reverse or prevent many of the issues associated with excess estrogen. This is important because LA has remarkable parallels to excess estrogen in terms of its metabolic and anti-health effects. You see, when you eat excess PUFA or LA, you increase your body's production of estrogen.
So, when you increase LA, estrogen levels go up — and that's not a good thing. Both LA and estrogen interestingly increase the flow of calcium from outside the cell to inside because the concentration of calcium outside as well is 50 times higher than inside. So, the excess as LA will cause the influx of calcium inside the cell, which causes nitric oxide and superoxide to increase inside the cell.
When you do this, with this magical combination, you increase a very pernicious reactive nitrogen species called peroxynitrite, and that causes pervasive damage to tissues in your body.
Both LA and estrogen also increase a potentially dangerous process in your body called lipolysis, which is simply the liberation of fatty acids from your fat cells into your bloodstream where they are mobilized. This then increases the oxidation or, simply, the burning of fats in your mitochondria, which is precisely what you want to avoid as ideally you want to be burning glucose in your mitochondria, not fatty acids.
Fortunately, vitamin E can help neutralize this damaging effect of LA. Vitamin E also directly inhibits the activity of an enzyme called aromatase. This is an enzyme that converts the male hormones like testosterone and DHEA into estrogens.
Even better, it serves as an estrogen antagonist, meaning it binds to the estrogen receptor to block it from binding to estrogen. This dramatically lowers the damage from excess estrogen.
Vitamin E works very similarly to the drug tamoxifen, which is used to treat estrogen receptor-positive breast cancers. For these reasons, I firmly believe nearly everyone needs to be getting vitamin E in their diet. However, due to the high LA burden, very few people are able to get enough vitamin E from their diet to suppress this oxidative destruction from excess LA in their tissues.
The good news is that since the supplementation is short term, you're not going to need it the rest of your life.
If you can keep your LA intake to below 5 grams a day for three years, it's likely you may not even need it at all, or at most, only a few times a month. However, if for whatever reason, during this time, or when the LA in your tissues are low or normal, and you go out and binge on a meal that's very high in LA, I would strongly recommend taking a vitamin E capsule to protect yourself from this exposure.
Vitamin E also protects against free radical damage and the normal effects of aging. It’s particularly important for brain health, and studies have found it can help delay the loss of cognitive function in people with Alzheimer’s disease by preventing cell membrane damage and neuronal death.1
How to Pick a Good Vitamin E Supplement

Most vitamin E supplements are synthetic. This is a major clue that
it is different from the vitamin E you're getting from real food.
How can you tell a vitamin E supplement is synthetic? Well, all you
must do is read the label. Fortunately, they make it pretty
simple.
Synthetic vitamin E is called alpha tocopherol acetate. The acetate is the key. If the label says tocopherol acetate, it's screaming that it is synthetic. Next, you need to pay attention to the orientation of the optical isomer. Most vitamin supplements are racemic, or they have left- and right-hand isomers. This is a problem as most biological molecules have optical isomers that are right-handed. They're usually called D and L isomers for right and left.
When you have both left and right isomers present, it’s called racemic. Biologically, there's usually only one optical isomer that works well, and with vitamin E it is the D isomer that works in your body, while the L isomer is useless. Yet in synthetic supplements, 50% of the vitamin E in the supplement is the useless L isomer.
To make matters even worse, many synthetic versions use an ester of vitamin E, which only has about 50% of the activity of the natural product. So, the total activity of many vitamin E supplements is reduced by 75%.
So, the first step in identifying healthy good vitamin E supplements is to make sure you're not getting real vitamin E and not synthetic. What you’re looking for is "d alpha tocopherol," as on the label below. As you can see on this label, it says that this is d alpha tocopherol. It is not DL or racemic; this is the pure D isomer, which is what your body can use.
You might also have noticed that this is vitamin E from sunflower oil, which has a very high percentage of LA. Not to worry, though, as the LA in the capsule is an insignificant amount, probably less than 50 or 100 milligrams.
Your goal is to keep LA intake under 5,000 milligrams, so it really won't negatively impact your LA intake at all. You'll also notice that the dose is 134 milligrams or units. You really wouldn't want to use much more than this, as it is unnecessary. More is not better; you don't want to take 400 units, you don't want 1,000 units, you want the sweet spot Goldilocks dose, which is about 100 units, or 100 mg.
You also see at the bottom of this label that there are other vitamin E isomers, the complete spectrum of tocotrienols, specifically the beta, gamma and delta types of vitamin E, which are also only the effective D isomer.
So, you can use this label as a template to select a healthy vitamin E supplement. It's important to get this right, and nearly everyone watching this would benefit from taking the appropriate vitamin E supplement, which is why I'm spending so much time on it.
Synthetic vitamin E is called alpha tocopherol acetate. The acetate is the key. If the label says tocopherol acetate, it's screaming that it is synthetic. Next, you need to pay attention to the orientation of the optical isomer. Most vitamin supplements are racemic, or they have left- and right-hand isomers. This is a problem as most biological molecules have optical isomers that are right-handed. They're usually called D and L isomers for right and left.
When you have both left and right isomers present, it’s called racemic. Biologically, there's usually only one optical isomer that works well, and with vitamin E it is the D isomer that works in your body, while the L isomer is useless. Yet in synthetic supplements, 50% of the vitamin E in the supplement is the useless L isomer.
To make matters even worse, many synthetic versions use an ester of vitamin E, which only has about 50% of the activity of the natural product. So, the total activity of many vitamin E supplements is reduced by 75%.
So, the first step in identifying healthy good vitamin E supplements is to make sure you're not getting real vitamin E and not synthetic. What you’re looking for is "d alpha tocopherol," as on the label below. As you can see on this label, it says that this is d alpha tocopherol. It is not DL or racemic; this is the pure D isomer, which is what your body can use.
You might also have noticed that this is vitamin E from sunflower oil, which has a very high percentage of LA. Not to worry, though, as the LA in the capsule is an insignificant amount, probably less than 50 or 100 milligrams.
Your goal is to keep LA intake under 5,000 milligrams, so it really won't negatively impact your LA intake at all. You'll also notice that the dose is 134 milligrams or units. You really wouldn't want to use much more than this, as it is unnecessary. More is not better; you don't want to take 400 units, you don't want 1,000 units, you want the sweet spot Goldilocks dose, which is about 100 units, or 100 mg.
You also see at the bottom of this label that there are other vitamin E isomers, the complete spectrum of tocotrienols, specifically the beta, gamma and delta types of vitamin E, which are also only the effective D isomer.
So, you can use this label as a template to select a healthy vitamin E supplement. It's important to get this right, and nearly everyone watching this would benefit from taking the appropriate vitamin E supplement, which is why I'm spending so much time on it.
10. Magnesium and Molecular Hydrogen
Magnesium
On the flip side, adequate magnesium levels help suppress the production of these inflammatory substances. Magnesium also helps activate your body's antioxidant defense systems, protecting your cells from oxidative stress and further reducing inflammation. Studies have shown that people with higher magnesium intake have lower levels of C-reactive protein, a key marker of inflammation. (Nutrients 2024)
By ensuring you're getting enough magnesium, you're not just supporting your energy production — you're also giving your body a powerful tool to combat chronic inflammation and reduce your risk of age-related diseases.
Molecular Hydrogen
PubMed has indexed more than 100 research studies on molecular hydrogen and anti-inflammatory.
In one human study, 20 patients with rheumatoid arthritis drank 0.5 L/day of hydrogen water for 4 weeks. By the end of the study, all patients with early rheumatoid arthritis achieved remission and
20% became symptom-free [R].
Other Anti-Inflammatory Nutrients
Other anti-inflammatory nutrients you may want to consider
include:
• Glycine — Glycine exerts potent anti-inflammatory effects by inhibiting activation of immune cells and suppressing the production of pro-inflammatory cytokines. It acts on inflammatory cells like macrophages to block the signaling of the NLRP3 inflammasome. Glycine also reduces TNFα, IL-6, and other cytokine levels in macrophages, and counteracts LPS-induced inflammatory responses. Furthermore, glycine acts on neutrophils to inhibit CXCR2 signaling and recruitment, as well as blocking ICAM-1 expression and limiting endothelial adhesion.
• Glycine — Glycine exerts potent anti-inflammatory effects by inhibiting activation of immune cells and suppressing the production of pro-inflammatory cytokines. It acts on inflammatory cells like macrophages to block the signaling of the NLRP3 inflammasome. Glycine also reduces TNFα, IL-6, and other cytokine levels in macrophages, and counteracts LPS-induced inflammatory responses. Furthermore, glycine acts on neutrophils to inhibit CXCR2 signaling and recruitment, as well as blocking ICAM-1 expression and limiting endothelial adhesion.
Related: 2023 Ceron et al - Glycine: The Smallest Anti-Inflammatory Micronutrient (PubMed)
• Boswellic acid — Boswellic acid, extracted from the boswellia serrata tree, has a long history of use in traditional medicine. It can reduce pain and inflammation throughout the body, including arthritis pain. (R)
• Green tea extract — Green tea extract contains a potent antioxidant catechin called EGCG, which combats inflammation, relieves joint and muscle soreness, and prevents future oxidative stress and damage. It can also improve the function of your brain, heart and blood vessels, and help your immune system fight off various diseases. (R)
• Boswellic acid — Boswellic acid, extracted from the boswellia serrata tree, has a long history of use in traditional medicine. It can reduce pain and inflammation throughout the body, including arthritis pain. (R)
• Green tea extract — Green tea extract contains a potent antioxidant catechin called EGCG, which combats inflammation, relieves joint and muscle soreness, and prevents future oxidative stress and damage. It can also improve the function of your brain, heart and blood vessels, and help your immune system fight off various diseases. (R)
Other Natural Ways to Reduce Inflammation?
Anti-Inflammatory Diet
Researchers have identified certain foods that can help
control inflammation. Many of them are found in the
so-called Mediterranean diet, which emphasizes fish,
vegetables and olive oil, among other staples.
There’s a standardized research tool that’s updated
regularly that allows anybody to see if they’re eating foods
we know cause chronic inflammation. This is called the
The Dietary Inflammatory Index or DII. The choices of pro-inflammatory foods were
initially based on studies showing that certain foods like
trans-fatty acids (unsaturated fats) caused a spike in serum
inflammatory markers in people.
A 2020 study published in the
Journal of the American College of Cardiology
(JACC), concluded that dietary patterns with a higher
pro-inflammatory potential were associated with higher CVD
risk. Reducing the inflammatory potential of the diet may
potentially provide an effective strategy for CVD
prevention.
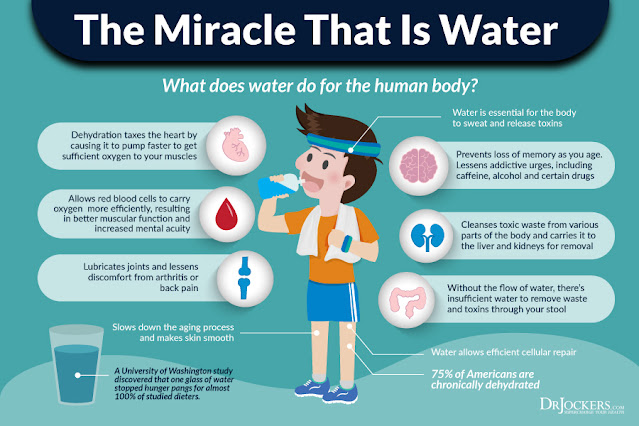
Hydration
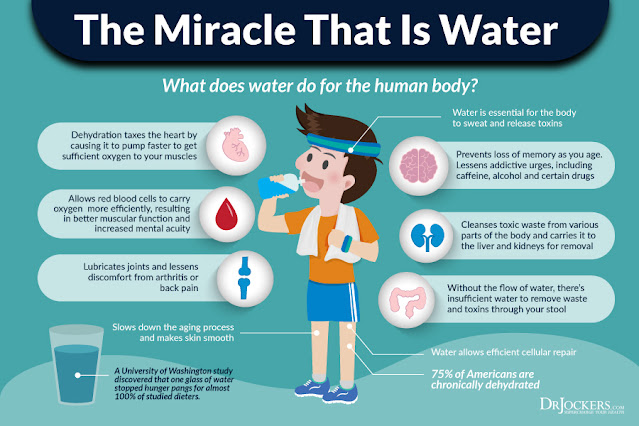
Exposure to toxins is one huge factor in chronic
inflammation. These could include pesticides, heavy
metals, air pollution, mold, and more. On a daily basis,
we are exposed to a list of toxins without even knowing
it. Hydrating effectively is one of the key strategies to
make sure the body is able to effectively detox.
Hydrating really well helps to clear out the bowels, keep toxins moving through the liver and kidneys, and
helps to eliminate them through sweat. Additionally,
your cells require adequate hydration to carry out proper
functions. In general, the more hydrated you are, the less
inflammation will be present in your body.
Autoimmune Protocol Diet
The Autoimmune Protocol (AIP) is a diet that aims to
reduce inflammation, pain, and other symptoms caused by
autoimmune diseases, such as lupus, inflammatory bowel
disease (IBD), celiac disease, and rheumatoid arthritis
(pubmed).
Many people who have followed the AIP diet report improvements in the way they feel, as well as reductions in common symptoms of autoimmune disorders, such as fatigue and gut or joint pain. Yet, while research on this diet is promising, it’s also limited.
The AIP diet is an elimination diet designed to help reduce inflammation or other symptoms caused by autoimmune disorders.
It’s comprised of two phases designed to help you identify and ultimately avoid the foods that may trigger inflammation and disease-specific symptoms. Research on its efficacy is limited but appears promising.
Due to its limited downsides, people with autoimmune disorders generally have little to lose by giving it a try. However, it’s likely best to seek guidance from a qualified health professional to ensure you continue to meet your nutrient needs throughout all phases of this diet.
Many people who have followed the AIP diet report improvements in the way they feel, as well as reductions in common symptoms of autoimmune disorders, such as fatigue and gut or joint pain. Yet, while research on this diet is promising, it’s also limited.
The AIP diet is an elimination diet designed to help reduce inflammation or other symptoms caused by autoimmune disorders.
It’s comprised of two phases designed to help you identify and ultimately avoid the foods that may trigger inflammation and disease-specific symptoms. Research on its efficacy is limited but appears promising.
Due to its limited downsides, people with autoimmune disorders generally have little to lose by giving it a try. However, it’s likely best to seek guidance from a qualified health professional to ensure you continue to meet your nutrient needs throughout all phases of this diet.
Choose My Plate
The Food Pyramid many of us grew up with has been replaced
with a colorful plate that emphasizes proper proportions.
One important message: Fill half your plate with vegetables.
Learn more at www.choosemyplate.gov.
Manage stress
Chronic stress contributes to inflammation. Meditation, yoga,
or guided imagery may help manage stress throughout the day.
Excerpt from The Disease Delusion - Dr Mark Hyman
Functional medicine is a personalized method for getting to
the root of symptoms and restoring balance. It is the story of
a little girl, Elise, who had suffered from intractable
psoriasis, with red, weeping, raw skin from head to toe, since
she was six months old. Her parents had taken her to the top
medical schools, and she had been given the most advanced
drugs, including powerful immune suppressants and chemotherapy
to shut off inflammation. When I first saw Elise she was four
years old. She had just emerged from a month in the intensive
care unit after fighting a life-threatening staphylococcus
infection triggered by her medication, Enbrel, which
suppressed her immune system. Rather than inquiring about the
root cause of her inflamed skin, doctors used medication to
suppress symptoms. Still she was no better. No one asked about
her diet or thought about how her history of antibiotics as a
baby affected her delicate gut flora, thus setting up the
conditions for inflammation.
Functional medicine led me to a different set of questions.
Rather than asking what drug I should use to treat the
symptoms, I asked what caused the inflammation in the first
place—a simple idea that is foreign to our medical training.
The causes of inflammation are few—microbes, allergens,
toxins, poor diet, stress. And I asked what her immune system
needed to regain balance. Then I applied these principles to
her by removing a common cause of inflammation in our
diet—gluten, known to be linked to psoriasis—and cleared out
bad microbes (yeast) in her gut that resulted from years of
antibiotics and steroids. I also added a few ingredients
needed to support proper immune function—omega-3 fats, zinc,
vitamin D, and probiotics to help balance her gut flora.
Within two weeks her skin, red and raw for over three years,
was clear. Not a miracle, but a repeatable result that is a
natural outcome of breaking our disease delusion and employing
a new framework for solving our chronic disease epidemic.
Key Takeaways
Anytime you see an article or health expert touting the best natural
anti inflammatory supplements or a one size fits all anti
inflammatory supplement, and they are recommending a specific
product(s) for everyone, buyer beware. This one size fits all
concept does not exist because we are all so biologically unique.
For example, someone who is experiencing chronic stress in addition to an exposure issue such as mercury or mold may benefit from glutathione more so than someone who has multiple viral infections and poor bone health. In that case, Vitamin D might be the front runner for this individual. One of the main reasons being that microbes can slow down immune reactivity by dysregulating the VDR receptor (Vitamin D receptor), ultimately to increase the host’s chance of survival.
For example, someone who is experiencing chronic stress in addition to an exposure issue such as mercury or mold may benefit from glutathione more so than someone who has multiple viral infections and poor bone health. In that case, Vitamin D might be the front runner for this individual. One of the main reasons being that microbes can slow down immune reactivity by dysregulating the VDR receptor (Vitamin D receptor), ultimately to increase the host’s chance of survival.
In summary, when combined with an anti-inflammatory diet, proper vitamin and mineral supplementation can be a true game-changer when it comes to fighting chronic inflammation. But, instead of going and buying every single supplement mentioned in this article, we encourage you to connect with a trusted functional medical practitioner to help you map out the best approach for your unique goals and health history.
Keep in mind that the best anti-inflammatory supplements will never mask poor sleep habits and a highly-processed diet.
References:

.png)

.png)






Comments
Post a Comment