I-PREVENT CANCER protocol: An Evidence-Based Guide to Cancer Prevention (2026 Edition)
Table of Contents — I-PREVENT CANCER Protocol (Best Diet and Cancer Fighting Supplements)
-
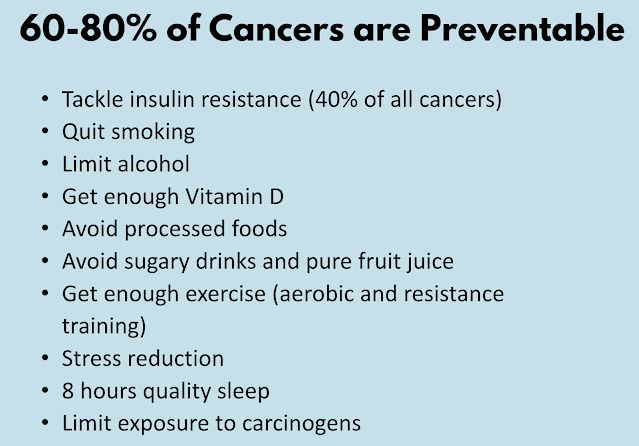
Introduction – Why preventive strategies matter and overview of the I-PREVENT framework
-
Methodology – How evidence was selected and interpreted
-
Causes of Cancer – Diet, lifestyle and biological contributors
-
Diet and Cancer – Nutrition and eating patterns for prevention
-
Lifestyle Recommendations – Alcohol avoidance, exercise, risk behavior modifications
-
Best Anti-Cancer Supplements – Individual supplement sections (in order of importance)
6.1. Vitamin D3, Vitamin K2 & Omega-3
6.2. Turmeric (Curcumin)
6.3. Vitamin C
6.4. Green Tea Extract (EGCG)
6.5. Probiotics & Garlic
6.6. Berberine
6.7. Magnesium
6.8. Molecular Hydrogen
6.9. Zinc -
Other Supplements & Natural Compounds Discussed – Additional agents referenced in context (e.g., melatonin, carotenoids)
-
Other Recommendations – Sleep quality, regular medical care, toxin avoidance
- Key Takeaways & Conclusion – Summary of the protocol’s holistic prevention strategy.
1. Introduction
Most of us recognize names like Val Kilmer (Batman Forever), Chadwick Boseman (Black Panther), Steve Jobs, Robin Gibb (Bee Gees), Donna Summer, Farrah Fawcett, Eartha Kitt, Peter Jennings, Paul Newman, Patrick Swayze, Sydney Pollack, Michael Crichton, Bob Denver, Ted Kennedy, Jerry Orbach, Anne Bancroft, William Rehnquist, and Tony Snow — just to name a few.
What do they all have in common? They each lost their lives to cancer.
In This Article:
- Methodology: Focuses on evidence-based research for cancer prevention and supplements.
- What is Cancer & Causes: Discusses how lifestyle and environmental factors contribute to cancer risk.
- Diet & Cancer Prevention: Plant-based (fruits, vegetables and whole grains), Mediterranean diets; avoid processed foods and processed red meat, sugar, and alcohol.
- Lifestyle & Cancer Prevention: Quit smoking, maintain healthy weight, exercise, reduce stress, and avoid radiation.
- Best Anti-Cancer Supplements: Includes Vitamin D3, Turmeric (Curcumin), Omega-3, Vitamin C, Green Tea Extract (EGCG), Probiotics and Garlic, Berberine, Magnesium, Molecular Hydrogen and Zinc.
- Other Recommendations: Quality sleep, regular medical care, avoiding toxins, infections, carcinogens.
- Key Takeaways: Focus on holistic and the combination of health, proper diet, supplements, and lifestyle changes.
AI tools like ChatGPT, Google's Gemini, and Microsoft's Copilot can be useful starting points for your inquiries, but they often provide generic answers that may lack the latest scientific depth and nuanced understanding you seek. Meanwhile, the vast amount of information available through the internet, social media, and AI can lead to information overload, with many conflicting facts and opinions making it difficult to discern what is accurate and applicable to your personal health or lifestyle. Despite the abundance of diet and lifestyle advice, this abundance can be overwhelming, and even doctors may sometimes struggle to help resolve lingering questions despite clear research findings.
Furthermore, the current state of AI in medical research and clinical use reflects both promise and limitations. While AI has great potential to aid in knowledge synthesis and clinical decision support, challenges persist such as algorithmic bias, limited robust clinical evidence, safety concerns, and the risk of automation bias where clinician skills may decline due to overreliance on AI. The integration of AI tools in biomedical research also raises concerns about reinforcement of common viewpoints over novel ideas and issues related to transparency and reproducibility. Therefore, while AI democratizes access to information, critical human judgment, wisdom, and careful interpretation remain essential to navigate complex and evolving scientific content effectively.
This perspective highlights that AI and online resources are valuable but limited tools that should be complemented by expert consultation and thoughtful evaluation of evidence, especially in complex fields like medicine and health.
 |
| Credit: Statista |
Breast, lung and colon cancer are among the most common, while the number of new cancer cases annually is expected to grow by more than 75% between 2022 and 2050.
Prevention is More Valuable Than Cure or Early Detection
Despite its importance, preventive measures often receive limited attention due to profit-driven motives. This is reflected in the scant coverage of preventive strategies in mainstream media.
The Ambiguity of Cancer Prevention
The realm of diet, lifestyle, and dietary supplements is often clouded with uncertainty. Without robust scientific evidence, the true potential of these options remains unclear. While your cancer specialist or oncologist may not delve deeply into these aspects during consultations, they can be crucial for your well-being.
Common Items with Uncommon Benefits
Many natural diet and supplement strategies can be found in everyday items available at your local supermarket. So why aren’t these strategies making headlines as the greatest cancer breakthrough of the 21st century?
Introducing the I-PREVENT CANCER Protocol
We are pleased to introduce the I-PREVENT CANCER protocol, designed to help individuals prevent cancer. This article serves as a consumer guide for cancer prevention, focusing on practical preventive strategies rather than technical theories. Our aim is to summarise relevant, updated, and practical points, providing you with a personal blueprint and resource for cancer prevention.
The name I-PREVENT was created in 2022 by the anonymous medical research team behind the website OneDayMD.com (the exact page you originally linked to). It is not an official protocol from any university, cancer center, or government health agency. Instead, it is a private, integrative/functional medicine-inspired framework that the OneDayMD authors built and branded themselves.
I – P – R – E – V – E – N – T
The authors designed it to stand for the seven pillars they consider most important for cancer prevention:
- Immune enhancement
- Polyphenols & phytochemicals
- Reduction of chronic inflammation
- Epigenetic modulation
- Vitamin optimisation
- Exercise & body composition
- Nutrient repletion (especially magnesium, zinc, omega-3)
- Toxins & hormone disruptors – avoidance
- 2022 – First published on OneDayMD as “Best Cancer Fighting Supplements 2022” and informally called the I-PREVENT protocol in the comments and follow-up posts.
- 2023–2024 – The same authors kept updating the page with newer studies and started explicitly branding it “I-PREVENT Cancer Prevention Protocol.”
- 2025 (latest major update) – The page was refreshed again in early 2025 with new meta-analyses, and the I-PREVENT name became the official header.
- It is not connected to the official “PREVENT” programs run by the National Cancer Institute or the MD Anderson PREVENT Cancer Preclinical Drug Development Program.
- It is not a registered trademark or a clinically validated protocol used in hospitals.
- It is a privately compiled, evidence-based summary created by physicians/researchers who practice functional and integrative oncology, intended for educational use.
2. Methodology
Case studies and preliminary results from small-scale human trials hold less significance than outcomes from umbrella reviews, systematic reviews and meta-analysis*, randomised controlled trials (RCTs), and more extensive, long-term human trials.
3. Causes of Cancer
- sustaining proliferative signaling,
- evading growth suppressors,
- resisting cell death,
- enabling replicative immortality,
- inducing angiogenesis, and
- activating invasion and metastasis.
- deregulating cellular energetics
- avoiding immune destruction
- Genome instability and mutation
- Tumor promoting inflammation
- unlocking phenotypic plasticity,
- non-mutational epigenetic reprogramming,
- polymorphic microbiomes
- senescent cells.
4. Diet and Cancer
If cancer hospitals are still serving french fries, potato chips, ice cream, and cakes, we are facing a serious problem.Cancer patients require carefully tailored nutrition to support their treatment and recovery. Healthy diets for cancer patients emphasize whole foods rich in fiber, lean proteins, healthy fats, fruits, and vegetables, while avoiding ultra-processed foods, fried snacks, and excessive sugars. Although some high-calorie treats like ice cream or cakes may be recommended occasionally to maintain weight in patients with poor appetite, regularly serving highly processed, nutrient-poor foods like french fries and potato chips contradicts best nutritional practices for cancer care.
 |
| Cancer-Causing Diet |
Leading cancer centers and dietitians recommend diets that help maintain strength, manage treatment side effects, support immune function, and reduce inflammation. This includes avoiding deep-fried and ultra-processed foods, limiting processed red meats, and focusing on nutrient-dense, minimally processed meals.
Ensuring cancer hospitals provide appropriate, evidence-based nutrition is essential to improving patient outcomes and quality of life during treatment.
1. The ACS 2020 Recommendation
- Foods that are high in nutrients in amounts that help achieve and maintain a healthy body weight;
- A variety of vegetables—dark green, red and orange, fiber-rich legumes (beans and peas), and others;
- Fruits, especially whole fruits with a variety of colors; and
- Whole grains.
- Red and processed meats;
- Sugar-sweetened beverages; or
- Highly processed foods and refined grain products.
2. A 2024 Update to ACS International Guidelines
- The review highlights the benefits of the Mediterranean diet in reducing cancer risk.
- Adherence to overnight fasting or carbohydrate consumption may contribute to cancer prevention, but excessive fasting may harm patients' quality of life.
- A vegetarian/pescetarian diet is associated with lower risks of general and colorectal cancer compared to a carnivorous diet.
- High heme and total iron intake are linked to increased lung cancer risk, while phytoestrogen intake is associated with reduced risk.
- Coffee and tea have a neutral impact on cancer risk.

|
|
|
3. Avoid Processed Foods and Sugar
Key findings of the study — Participants came from the general adult population, which included both men and women with diverse dietary patterns and health backgrounds. Over a follow-up period that averaged 7.57 years, the researchers recorded new cancer diagnoses and compared them against levels of preservative intake. The findings were clear — people who consumed more preservatives had higher rates of overall cancer and breast cancer. This association remained after accounting for factors such as age, body weight, physical activity, smoking, alcohol intake, and overall diet quality.
4. Plant Based Diet and Mediterranean Diet
5. Dietary Fiber
Investigators compared individuals who regularly ate ample amounts of fiber — often exceeding the typical intake recommended by many national guidelines — to those whose eating habits were comparatively low in fiber.
Some of the analyses concentrated on populations that were already at higher risk for malignancies, while others looked at generally healthy adults who maintained diverse diets. The researchers behind this umbrella review looked for consistent patterns across different age groups and geographic regions.
They came away with a strong conclusion: the more fiber people consumed, the lower their chance of developing certain cancers, especially gastric, esophageal, ovarian and endometrial tumors.
Investigators noted that in several meta-analyses, people with higher fiber consumption had a reduced likelihood of gastric cancer. Gastric refers to your stomach itself, and these findings are especially notable since stomach cancers often go unnoticed until they are advanced. The authors emphasized that even moderate increases in total daily fiber showed a measurable shift in the overall incidence of gastric tumors.
The authors also revisited a handful of studies about breast cancer. Those showed that greater fiber ingestion tracked closely with fewer instances of tumor growth, especially in postmenopausal individuals. One explanation offered across several discussions within the umbrella review was that dietary fiber might reduce estrogen reabsorption.
By preventing excessive hormone recirculation, fiber could help maintain balanced hormone levels, thus diminishing the conditions under which abnormal breast cells would flourish.
Beyond these disease-specific details, some of the meta-analyses examined an intriguing aspect of how fiber moderates inflammation. When inflammation runs rampant, it feeds the growth of malignant cells in various tissues. While the reviewed papers did not universally measure inflammatory markers, a few singled out fiber's ability to keep inflammation in check.
6. Fasting, Calorie Restriction, Low-Carb Diet and Keto Diet (Controversial)
You’ve probably read online that fasting, low-carb diets, and keto diets can reduce your risk of cancer. We’ve included this topic due to its popularity, but after analyzing various available evidence, the conclusion remains mixed. That’s why we’ve labeled this recommendation as ‘controversial.’Thomas N. Seyfried, a well-known scholar in cancer research and a Professor of Biology at Boston College, believes the existing cancer treatment system is “broken.” He said once people understand the metabolic theory of cancer, treatments like chemotherapy and radiotherapy will be replaced by new treatments.
The ketogenic diet is adopted because cancer cells have defective mitochondria and impaired metabolism, so they can only rely on fermented sugars and glutamine* (see below) for energy. Cancer cells cannot obtain energy from ketone bodies as ketone bodies cannot be fermented. As for cells with normal metabolic function, they can obtain energy by metabolizing ketone bodies [Nature 2019].
Diet diversity also plays a key role. Constantly eating the same macronutrient balance can make metabolism rigid, whereas cycling between carbohydrate-rich and fat-based fuel periods—through time-restricted eating, low-carb days, or occasional fasting—encourages cells to remain metabolically flexible. For most people, there’s no need for extreme diets. It’s about training your metabolism to handle both abundance and scarcity.
Food quality also matters. “Poor nutrition may play a role in creating tumor-friendly environments—pushing cells into stress and making them more likely to become malignant,” Mona Jhaveri, who has a doctorate in biochemistry and molecular biology, said. Persistently high blood sugar and chronic inflammation from ultra-processed foods and refined sugar can damage mitochondria and promote the same metabolic inflexibility in which cancer thrives.
Key Takeaway: Avoid sugar, processed foods and red meat.
7. Coffee and Cancer
8. Tattoos, Chemical Hair Straighteners and even Hot Tea linked to Cancer
Keep in mind that none of these factors has evidence on par with risks like drinking alcohol or smoking. That said, here are five surprising things that have been associated with developing cancer — and what you should know about them.
1. Tattoos
2. Hookah smoking (aka Shisha)
3. Very hot beverages
4. Chemical hair straighteners and dyes
5. Meats cooked at high temperatures
9. Can the raw food diet prevent cancer?
5. Lifestyle and Cancer Prevention
1. Avoid tobacco
Smoking is a major cause of cancer. Cigarette smoking topped the charts as the leading risk factor, contributing to nearly 20 percent of all cancer cases and close to 30 percent of cancer deaths. Smoking comprised 56 percent of potentially preventable cancers in men and almost 40 percent of those in women (Journal of the American Cancer Society 2024)But it's not only smoking that's harmful. Chewing tobacco has been linked to cancer of the mouth, throat and pancreas.
Staying away from tobacco — or deciding to stop using it — is an important way to help prevent cancer. For help quitting tobacco, ask a health care provider about stop-smoking products and other ways of quitting.
2. Maintain a healthy weight and be physically active
Physical activity counts too. Besides helping control weight, physical activity on its own might lower the risk of breast cancer and colon cancer.
Doing any amount of physical activity benefits health. But for the most benefit, strive for at least 150 minutes a week of moderate aerobic activity or 75 minutes a week of hard aerobic activity.
You can combine moderate and hard activity. As a general goal, include at least 30 minutes of physical activity in your daily routine. More is better.
Results of the first randomized controlled trial of exercise as a treatment for recurrent high-risk cancer were presented at the American Society of Clinical Oncology's (ASCO) annual meeting in Chicago on June 1, 2025, and they stunned the crowd of doctors gathered there from around the world.
The 17-year trial (NEJM 2025) included over 880 patients from around the globe, each recovering from high-risk stage 2 or stage 3 colon cancer after treatment. Half of the participants were given general advice about exercise and how it can improve cancer survival. The other half were given a structured, three-year exercise prescription to follow, with the goal of preventing recurrence or a new cancer diagnoses.

In the trial, exercise outperformed what adjuvant (or, secondary) chemotherapy can do to boost a patient's long-term survival, after surgery and primary treatment is over. Adjuvant cancer treatment is the kind designed to kill any extra cancer cells left behind, and prevent cancer from coming back.
“Compared with undertaking no resistance training, undertaking any amount of resistance training reduced the risk of all-cause mortality by 15% ... cardiovascular disease mortality by 19% ... and cancer mortality by 14% ...
A dose-response meta-analysis of 4 studies suggested a nonlinear relationship between resistance training and the risk of all-cause mortality. A maximum risk reduction of 27% was observed at around 60 minutes per week of resistance training ... Mortality risk reductions diminished at higher volumes.”
3. Avoid Alcohol
6. Best Cancer Fighting Supplements: Evidence Based Review
1. Vitamin D3 and K2
- This large-scale review looked at diverse populations — The data covered various groups and nationalities, including women in the U.S. Midwest, Danish adults with a family history of cancer and Canadians living in high-altitude areas. The participants had different health statuses as well — some had colorectal cancer, or a documented vitamin D deficiency. Others were also given a vitamin D supplement.
- While the participants varied in health status and genetic risk, a consistent pattern emerged — The researchers found that the lower your vitamin D levels, the higher your risk of developing colon cancer. On the flip side, people with adequate or optimal levels of vitamin D had dramatically lower rates of cancer.
- Unfortunately, majority of people today have very low levels of this vital nutrient — A recent study that looked at the vitamin D status of more than 5,600 adults found that 37.6% had vitamin D insufficiency (blood levels between 20 and 30 ng/mL), while 42% were severely deficient (blood levels lower than 20 ng/mL) in this nutrient.
- A landmark 1996 study found that women with the highest vitamin D intake had a 58% lower risk than those with the lowest intake.
- A 2021 meta-analysis found a 39% lower risk of colorectal cancer in people with higher blood levels of vitamin D. The researchers also noted that when vitamin D levels were monitored over time, those who maintained higher levels had a 20% lower chance of developing colorectal cancer down the line.
- A Canadian study found that supplementing with vitamin D reduced the incidence of precancerous polyps — by 33% for all polyps and 43% for high-risk ones. These polyps often go on to become cancer if not addressed early, so this kind of intervention has massive implications.
- The Iowa Women's Health study found that women who took vitamin D with calcium saw a 15% drop in colorectal cancer risk compared to those who didn't take any supplements.
- The Danish "Diet, Cancer and Health" study (one of the major ones included) found that vitamin D offered even stronger protection in people with a high genetic risk of colon cancer. That means if you've got a family history of this disease, optimizing your vitamin D status isn't just helpful — it could be life-saving.
Research has shown that once you reach a minimum serum vitamin D level of 40 ng/mL (100 nmol/L), your risk for cancer diminishes by a whopping 67%, compared to having a level of 20 ng/mL or less.
However, if you find supplementation is necessary after a serum vitamin D test, also supplement with magnesium and vitamin K2 (MK-7) to ensure proper balance. You'll also want to ensure you're following an overall healthy lifestyle to reduce your cancer risk as much as possible.
2. Turmeric (Curcumin)
Unfortunately, while there's some curcumin in whole turmeric, there's not enough in the regular spice to achieve clinically relevant results. The turmeric root itself contains only about 3% curcumin concentration. Another major limitation of curcumin as a therapeutic agent is that it is poorly absorbed. When taken in its raw form, you're only absorbing about 1% of the available curcumin.
3. Fish Oil (Omega-3 Fatty Acids)
Make sure you buy high-quality omega-3 fatty acid supplements, meaning that the omega-3 fatty acids are pure and have not oxidized much (having low “TOTOX” value).
TOTOX value stands for total oxidation value. The omega 3 fatty acids EPA and DHA from fish oil are highly sensitive to oxidation. This means that they are rapidly affected by contact with oxygen. Oxidised fatty acids are not beneficial to our health. For this reason, a good fish oil supplement has a low TOTOX value. The maximum TOTOX value is set at 26 by the Global Organization for EPA and DHA omega-3.
4. Vitamin C
Synthetic Ascorbic acid is NOT the same as whole food or whole fruit vitamin C*.
Whole food vitamin C can also boost your copper level, as vitamin C contains an enzyme called tyrosinase, which has 2 atoms of copper in it. Ascorbic acid is prooxidant, while vitamin C complex is actually an antioxidant. Anything that has copper is going to be antioxidant.
5. Green Tea (EGCG)
A 2012 study examined the relationship between smoking, green tea consumption, and lung cancer risk in 170 primary lung cancer cases and 340 healthy controls.
The findings were striking: smokers who never drank green tea had a 13.16-fold greater risk of developing lung cancer compared to smokers who drank more than one cup of green tea daily (OR = 13.16, 95% CI = 2.96–58.51).
This translates into a 92.4% reduction in the chance of getting lung cancer if a smoker chose to drink at least one cup of green tea per day.
6. Melatonin
7. Garlic (Allicin) and Aged Garlic Extract
One study of 543,220 participants found that those who ate lots of Allium vegetables, such as garlic, onions, leeks and shallots, had a lower risk of stomach cancer than those who rarely consumed them (Source).
Another study of 471 men showed that a higher intake of garlic was associated with a reduced risk of prostate cancer (Source).
Several clinical studies have found an association between garlic intake and a lower risk of certain types of cancer.
In a 2004 study, researchers conducted the largest cancer prevention trial ever done with garlic extract involving some 5000 participants. They gave half the participants this natural agent for just one month per year over three years, then followed them for five more years.
The results were stunning: garlic extract reduced stomach cancer incidence by 52%, with the strongest effect in men. This isn’t a small effect—this is comparable to or better than many cancer drugs.
In a 2019 study, researchers published a 22-year follow-up data in a prestigious medical journal (BMJ). Even 17 years after people stopped taking this supplement, they still had 34% lower cancer mortality. Think about that: a natural compound you take for three years continues protecting you nearly two decades later.
How does garlic extract do this? Unlike most supplements that work through one pathway, it’s like a Swiss Army knife—it attacks cancer through multiple mechanisms simultaneously. These involve suppressing cancer stem cell pathways, activating autophagy and supercharging the immune system.
- First, it reduces insulin-like growth factor-1 (IGF-1), which cancer cells need to grow.
- Second, it activates autophagy—the same process Guy’s 42-day fast triggered.
- Third, it suppresses a master switch called NFκB that controls inflammation and cancer stem cell survival.
- Fourth, it enhances Natural Killer (NK) cells—your immune system’s assassins that hunt down cancer cells—by up to 300%.
Where to Buy Aged Garlic Extract: Kyolic Aged Garlic Extract Formula 100 (Amazon)
8. Magnesium and Molecular Hydrogen
An analysis of the prospective, Swedish Mammography Cohort (JAMA 2005), evaluated 61,433 women aged 40 to 75 without a history of cancer for a mean follow-up of 14.8 years. The highest quintile of magnesium intake was associated with a significantly lower risk of CRC compared with the lowest quintile. This benefit was observed for both colon and rectal cancers.
A case-control study evaluated 2204 subjects from the Tennessee Colorectal Polyp Study (2007), which demonstrated that increasing total magnesium intake was significantly associated with decreasing risk of CR.. The highest tertile of dietary magnesium intake (>298 mg/day) was significantly associated with reduced risk of CRC in an age-adjusted model.
A study of 140,601 postmenopausal women from the Women’s Health Initiative (2015) with an mean follow-up of 13 years demonstrated a significant reduction in CRC risk with the highest quintile of total magnesium intake compared with the lowest quintile of magnesium intake. The benefit was driven by colon cancer, with a trend for rectal cancer.
Magnesium and Pancreatic Cancer
A study of 66,806 subjects aged 50 to 76 at baseline from the Vitamins and Lifestyle cohort (Nature 2015) evaluated magnesium intake and the incidence of pancreatic cancer during a mean follow-up of 6.8 years. Subjects with magnesium intake below the recommended dietary allowance were more likely to develop pancreatic cancer, particularly in those whose intake was less than 75% of the recommended dietary allowance. In this study, a 100 mg/day decrease in magnesium intake resulted in a 24% increase in risk of pancreatic cancer.
9. Zinc and Cancer
10. Gut Microbes and Probiotics
Certain gut bacteria also promote inflammation, which is an underlying factor in virtually all cancers, whereas other bacteria quell it. The presence of certain gut bacteria has even been shown to boost the patient's response to anticancer drugs. (Nature 2018)
One way in which gut bacteria improve the effectiveness of cancer treatment is by activating your immune system and allowing it to function more efficiently. Researchers have actually found that when these specific microbes are absent, certain anticancer drugs may not work at all.
11. Berberine
In a 6-Year follow-up of a randomized clinical trial, published in 2025 (Cell Reports Medicine), the protective effects of berberine persist for at least 6 years after treatment cessation, with lower adenoma recurrence rate (34.7% vs. 52.1%) and lower neoplasm occurrence rate (63.4% vs. 71.0%). The authors concluded that berberine may serve as a potential long-term preventive agent against adenoma recurrence after polypectomy.
12. Quercetin
2022 - A paper published in August 2022 in Nutrition Research analyzed the pro-apoptotic effect that quercetin has on aging cells. The paper reviewed preclinical and early phase data using quercetin as a senolytic agent and found the data showed it was effective in “preventing or alleviating cancer formation.”
The authors reviewed the importance of cellular aging in the development of cancer cells and the effect that quercetin may have on the suppression of cancer cell proliferation.
Cellular senescence is a dynamic and multi-step process that is associated with alterations in metabolic activity and gene expression. This can compromise tissue regeneration and contribute to aging. On the other hand, by removing senescent cells, age-related dysfunction can be attenuated and potentially extend the lifespan.
13. Carotenoids (α-carotene, β-carotene, β-cryptoxanthin, lutein, zeaxanthin, and lycopene)
14. Nicotinamide
In this retrospective study of 33 822 veterans, published in JAMA Dermatology (2025), there was a decreased risk of 3 types of skin cancer associated with use of nicotinamide. The magnitude of reduction was associated with the number of skin cancers before nicotinamide use.15. Beta-Glucans
Related: The Cancer Risk Reduction Protocol to reduce Risk by 95%? (Dr Justus Hope)
Can Antioxidant Supplements help Prevent Cancer?
It is possible that the lack of benefit in clinical studies can be explained by differences in the effects of the tested antioxidants when they are consumed as purified chemicals as opposed to when they are consumed in foods, which contain complex mixtures of antioxidants, vitamins, and minerals (Source).
Can Supplements Lead to an Increased Risk of getting Cancer?
7. Reduce and Optimise Stress
8. Quality Sleep
9. Other Cancer Prevention Strategies
Get Regular Medical Care and Health Screening
Doing regular self-exams and having screenings for cancers — such as cancer of the skin, colon, cervix and breast — can raise the chances of finding cancer early. That's when treatment is most likely to succeed. Ask a health care provider about the best cancer screening schedule for you.
Avoid exposure to environmental toxins and infections that contribute to cancer
Avoid unnecessary exposure to Radiation and EMF (ElectroMagnetic Field)
Avoid risky behaviors
- Practice safe sex. Limit the number of sexual partners and use a condom. The greater the number of sexual partners in a lifetime, the greater the chances of getting a sexually transmitted infection, such as HIV or HPV.
- People who have HIV or AIDS have a higher risk of cancer of the anus, liver and lung. HPV is most often associated with cervical cancer, but it might also increase the risk of cancer of the anus, penis, throat, vulva and vagina.
- Don't share needles. Injecting drugs with shared needles can lead to HIV, as well as hepatitis B and hepatitis C — which can increase the risk of liver cancer. If you're concerned about drug misuse or addiction, seek professional help.
Key Takeaways
- Diet and Lifestyle strategies should be part of a comprehensive broad multi-modal approach to cancer prevention that may also include other interventions. Each individual’s needs and responses to different approaches will vary, making it essential to consider a combination of options and several strategies for optimal outcomes. That said, there is no single miracle approach alone that can prevent all cancers for everyone.
- You could also complement your research and read more from the American Cancer Society site. The site has comprehensive information on cancer. You could read more on cancer prevention by cancer type here: http://www.cancer.gov/cancertopics/prevention
- For more information on treatment, causes and prevention, screening and research, check out this comprehensive resource page (by cancer type): https://cancer.aestheticsadvisor.com/p/cancer-types-by-system.html.
- For information on diet and lifestyle for cancer survivors, check out: I-TREAT Cancer Protocol: Diet and Lifestyle Guide For Cancer Survivors.
Disclaimer
- Although this is a comprehensive guide, please do not consider this guide as personal medical advice, but as a recommendation for use with professional providers. Consult with your doctor and discuss with her/him.
- Our aim here isn't to replace your doctors' advice. It is intended as a sharing of knowledge and information. Do take note that most strategies are not 100% protective against cancer. It's a continuous struggle between the immune system and the cancer cells.
- Gendicine, The First Approved p53 Gene Therapy Product for Cancer: 20 Years Track Record
- I-LONGEVITY Protocol: Anti Aging and Longevity Protocol (2025 Edition)
Feel free to share or post your comments below.
The Wellness Company's Base Spike Detox Trio
This base spike protein detox protocol consists of these three powerful ingredients: Spike Support's Nattokinase, Bromelain, and Tumeric Extract. Vaccinated or not, prioritizing your well-being has never been more crucial.
Buy this ultimate detox bundle today, researched by Dr. Peter McCullough.
Recommended to maintain daily health for anyone exposed to COVID, vaccines, or shedding – and may help your body repair itself and remain at optimal health.








.png)

.png)
.png)






Dr Mercola would debate the evil of sunshine. Eatting a good whole food and meat diet with morning or evening sun will give the natural vt D you need. covid-19 problem solved.
ReplyDelete