Top 20 Alternative Cancer Treatments that Work: Evidence Based (2026 Edition)
This is a review of the published literature showing options for natural strategies and repurposed drugs that can be used in cancer prevention and treatment. It is not intended as a stand-alone guide to treating cancer. Nothing in this document should be taken as a basis to initiate treatment without guidance or avoid any treatment prescribed by your treating physician. This information is offered as a basis to assist mutual decision-making.

|
| Diverse cancer hallmarks targeted by repurposed non-oncology drugs. This figure was created with Biorender.com. Source: Nature 2024 |
Methodology
Top Alternatives and Metabolic Interventions to Control Cancer
The Repurposing Drugs in Oncology (ReDO) project has cataloged 372 approved drugs with anticancer effects. It would be impossible to review all the drugs in ReDo’s database in this article; rather, we have focused on, curated and evaluated the drugs or natural compounds that appear to have the greatest clinical utility. These repurposed drugs are listed in priority according to the strength of the supporting clinical and mechanistic evidence.SUMMARY OF TOP REPURPOSED DRUGS, METABOLIC INTERVENTIONS AND COMPLEMENTARY MEDICINE TO CONTROL CANCER
1. Ivermectin and Cancer
Ivermectin and its potential role in cancer treatment have sparked significant interest online. Through our research, we've observed that most studies available are preclinical, with a notable lack of published clinical studies. To assist with further investigation, we have compiled and categorized case reports by cancer type in one place.
While conventional medical professionals often regard case reports as anecdotal or lower-quality evidence, they generally prioritize large, double-blinded, randomized placebo-controlled trials (RCTs) as the gold standard. We acknowledge that RCTs provide stronger evidence.
Still, the potential benefits of Ivermectin, coupled with its comparatively low risk profile and cost, warrant serious consideration and further exploration.When this occurs in Stage 1, 2, or 3 cancers, it is sometimes difficult to tell whether it was the standard treatment, that is the surgery, chemotherapy, radiation or immunotherapy that produced the benefit. However, when the cancer has progressed to Stage 4, and particularly when it involves one of the often-incurable cancers such as the types in the below table under the “Palliation Only (Metastatic)” category where standard chemotherapy is largely ineffective, it becomes obvious that the repurposed drug made the difference.
The anti-parasitic dosage is not as effective for people looking for a dosage against cancer. Dosage will need to be adjusted according to cancer type and stage.
Ivermectin dosage should be based on ivermectin cancer studies. Multiple factors are considered including studies including ivermectin for cancer, anecdotal studies and case series, the aggressiveness of the cancer type and the cancer stage.
Cancer dosage estimation can be adjusted based on the time that a person has to beat cancer or its risk to the patient - this includes both the cancer type and whether the cancer has spread or metastasised.
Some cancers provide the patient with less time to beat the cancer e.g. fast growing cancer, and of course; metastasis also means that the time to beat the cancer is shorter than before metastasis.
2. Fenbendazole / Mebendazole / Albendazole and Cancer
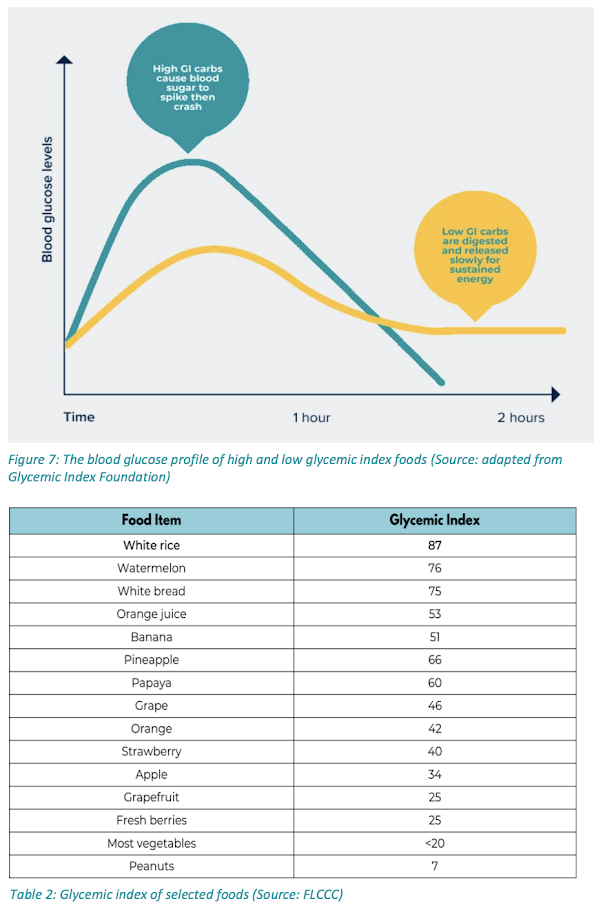
3. Best Diet for Cancer Treatment
*Red meat is one of the highest sources of glutamine (1.2 g glutamine per 100 g serving) (Healthline).
Key Takeaway: Avoid sugar, processed foods and red meat.
The Cholesterol-Saturated fatty acid hoax began to proliferate in the 1960s. Dr. Ancel Keys popularized the notion that saturated fats and high cholesterol were the primary causes of atherosclerotic heart disease — the so-called Diet-Heart Hypothesis. This concept has been vigorously studied, including in many randomized controlled trials, and has been convincingly proven to be false (BMJ 2016). Indeed, replacing saturated fats with a diet high in vegetable oils (linoleic acid) was associated with higher rates of death, cardiovascular and coronary heart disease as well as a significantly increased risk of cancer (BMJ 2013).
One of the reasons for this is because ketogenic diets increase the stress hormones — cortisol, glucagon and adrenaline. On the other hand, one of the reasons why ketogenic and carnivore diets are usually helpful for a time is because, if implemented properly, you’re radically reducing your intake of omega-6 fats, linoleic acid (LA) in particular, which is one of the primary drivers of ill health.
Dr. Jason Fung, a nephrologist and fasting expert, however, would argue that fasting is a purposeful way of managing one’s day by allocating specific times for eating.
The benefits of fasting can vary among individuals, and the preferred type of fasting can also differ. Intermittent fasting is generally safe, but not everyone responds well to prolonged fasting.
During prolonged fasts, the body primarily breaks down fat for energy rather than muscle. However, the extent to which fat or muscle is targeted can vary based on an individual’s body composition. Those who have more fat to lose may lose more fat and less muscle, while those with higher muscle mass may experience a greater breakdown of protein stores.
Studies have shown that lean muscle mass loss occurs within the first day of prolonged fasting, regardless of an individual’s fat and muscle proportions. Therefore, individuals with significant muscle mass may experience more muscle loss and less fat loss during prolonged fasting.
There are different approaches to incorporating fasting into one’s lifestyle, such as intermittent fasting or longer fasting periods every few months. Social norms, like having dinner together, can discourage extended fasting, so it’s important to choose a fasting style that suits one’s lifestyle and preferences.
However it should be noted that intermittent fasting is not recommended for:
- Older people and patients on chemotherapy are notorious for getting frail very quickly if they skip even one meal. They don’t eat very often, but they need their meal. If you don’t give it to them, they can very quickly decline.
- Extended fasting is also not a healthy long term strategy as it increases your stress hormones and worsens mitochondrial function.
- People with diabetes and kidney disease are also recommended to check with their primary care physicians before considering intermittent fasting.
- Those taking hypoglycemic or antihypertensive medication are particularly at risk, as they may end up overdosing. If you're on medication, you need to work with your doctor to ensure safety, as some medications need to be taken with food and/or can become toxic when your body chemistry normalizes.
- People younger than the age of 18, as it can prevent growth.
- Pregnant and breastfeeding women are also not recommended to fast intermittently.

|
| Credit: FLCCC 2024 Conference |
4. Vitamin D3, Omega 3 and Cancer
- fatty fish
- egg yolks
- fortified milk

|
| Summary of the anti-cancer pathways of the repurposed drugs and nutraceuticals |
- Supplementation: Dose titration according to vitamin D blood levels, aiming for a level of > 50 ng/mL (target 55-90 ng/mL)
- Sun Exposure: Safe sunlight exposure can naturally boost vitamin D levels.
- Synergy: Vitamin D3 works well with vitamin K2 and magnesium. Make sure to take 500 mg to 1000 mg of magnesium and 150 mcg of vitamin K2, (not K1) which are important cofactors for optimizing vitamin D function.
Consideration and Caution
5. Turmeric (Curcumin) and Cancer
Turmeric and black pepper each have health benefits, due to the compounds curcumin and piperine. As piperine enhances curcumin absorption in the body by up to 2,000%, combining the spices magnifies their effects. (Healthline)
Curcumin in Combination with Immunotherapy
Immunotherapies such as immune checkpoint inhibitors (ICIs), cancer vaccines, and adoptive cell therapies have minimised the shortcoimngs of traditional conventional cancer therapies and revolutionized the landscape of cancer therapeutics by offering improved side effects and lasting responses in many patients. (Cancers 2025)Listeria-MAGE-B is a vaccination that is primarily used to treat breast cancer by inhibiting IL-6. This vaccine works by targeting IL-6, which is particularly high in breast cancer and is associated with immunosuppressive effects in the TME. Curcumin was shown to be a good adjuvant for this vaccine by targeting by boosting T-cell responses and further inhibiting IL-6 production. The mechanism by which curcumin reduces the production of IL-6 is through its interference with STAT3 pathways. The response of CD4 and CD8 T cells was shown to improve when curcumin was used alongside the vaccination.
Given curcumin’s ability to attack many aspects of cancer and modulate the immune cells within the TME, it may be useful as an adjuvant in cancer vaccine therapies. As cancer vaccines continue to evolve and progress, further studies should explore curcumin in combination with the therapy. (Cancers 2025)
6. Magnesium and Molecular Hydrogen
An analysis of the prospective, Swedish Mammography Cohort (JAMA 2005), evaluated 61,433 women aged 40 to 75 without a history of cancer for a mean follow-up of 14.8 years. The highest quintile of magnesium intake was associated with a significantly lower risk of CRC compared with the lowest quintile. This benefit was observed for both colon and rectal cancers.
A case-control study evaluated 2204 subjects from the Tennessee Colorectal Polyp Study (2007), which demonstrated that increasing total magnesium intake was significantly associated with decreasing risk of CR.. The highest tertile of dietary magnesium intake (>298 mg/day) was significantly associated with reduced risk of CRC in an age-adjusted model.
A study of 140,601 postmenopausal women from the Women’s Health Initiative (2015) with an mean follow-up of 13 years demonstrated a significant reduction in CRC risk with the highest quintile of total magnesium intake compared with the lowest quintile of magnesium intake. The benefit was driven by colon cancer, with a trend for rectal cancer.
Magnesium and Pancreatic Cancer
A study of 66,806 subjects aged 50 to 76 at baseline from the Vitamins and Lifestyle cohort (Nature 2015) evaluated magnesium intake and the incidence of pancreatic cancer during a mean follow-up of 6.8 years. Subjects with magnesium intake below the recommended dietary allowance were more likely to develop pancreatic cancer, particularly in those whose intake was less than 75% of the recommended dietary allowance. In this study, a 100 mg/day decrease in magnesium intake resulted in a 24% increase in risk of pancreatic cancer.
7. Vitamin C, Aspirin and Celecoxib (Celebrex)
The study compiled results from 118 observational studies involving approximately 1 million cancer patients. It revealed that daily intake of low-dose aspirin (75 or 81 milligrams) was associated with a 21 percent reduction in all-cause mortality.
A study involving pancreatic cancer patients undergoing surgery indicated that patients who took aspirin had a three-year survival rate of 61.1 percent, compared to 26.3 percent for those who did not take it.
The researchers conducted a comprehensive analysis of all observational studies on aspirin and digestive tract cancers published until March 2019, encompassing over 150,000 cases. The results revealed that, compared to patients not using aspirin, those who regularly took aspirin had a 27 percent reduced risk of colorectal cancer, a 33 percent reduced risk of squamous cell esophageal cancer, a 39 percent reduced risk of adenocarcinoma of the esophagus and gastric cardia, a 36 percent reduced risk of stomach cancer, a 38 percent reduced risk of hepatobiliary tract cancer, and a 22 percent reduced risk of pancreatic cancer. However, there was no significant change in the risk of head and neck cancer.
For colorectal cancer, taking a daily dose of aspirin between 75 and 100 milligrams can reduce the risk by 10 percent, while a daily dose of 325 milligrams can reduce the risk by 35 percent.
In laboratory tests, the aspirin-vitamin C combination showed a strong cytotoxic effect on liver cancer cells but was much less harmful to normal lung cells. This selectivity is crucial for reducing the side effects associated with cancer treatments. The synergy between these two common substances appears to enhance their individual anticancer properties, offering a safer alternative to harsh chemotherapies.
The potential of aspirin and vitamin C extends beyond the lab, with encouraging results in animal studies. When tested on rats with chemically induced liver cancer, the combination therapy showed remarkable results. After 90 days of treatment, the livers of treated rats had significant improvement in both appearance and function.
This synergistic effect likely stems from combining aspirin's anti-inflammatory properties with vitamin C’s potent antioxidant capabilities. The two compounds appear to work together to create a more hostile environment for cancer cells, impeding their growth and proliferation.
By attacking tumors through multiple mechanisms simultaneously, the aspirin-vitamin C combination may overcome some of the adaptations cancer cells typically develop to evade single-compound treatments.
Beyond just shrinking tumors, the aspirin-vitamin C combination significantly extended survival times and appeared to improve overall health in the tumor-bearing mice. Mice treated with the combination survived an average of 93.5 days, compared to just 54 days for untreated tumor-bearing mice — a 73% increase in lifespan.
8. Metformin
A search on PubMed for “metformin AND cancer” yielded more than 7,000 citations.Numerous trials have shown that metformin, routinely used to treat diabetes, also inhibits the development of cancer cells and reduces cancer cell proliferation. Unlike most standard chemotherapy, metformin suppresses cancer stem cells, the root of cancer. (Shi 2017)
Meta-analyses have examined the role of metformin in the primary prevention of cancer, where it was found to significantly reduce overall cancer incidence (Gandini 2014). Lega et al (2014) performed a meta-analysis of 21 observational studies, evaluating the outcomes of diabetic patients with cancer who were receiving metformin. In this study, metformin was associated with a reduction in all-cause mortality and cancer-specific mortality; patients with colorectal cancer demonstrated the greatest benefit.
- AMPK Activation: Leads to downstream mTOR inhibition, reducing cell growth.
- mTOR Inhibition: Limits cancer cell survival and proliferation.
- Insulin/IGF Signaling Reduction: Lowers circulating growth factors that fuel metastasis.
- Metabolic Reprogramming: Alters cancer cell energy metabolism.
9. Melatonin
A case report from the Department of Pathology and Laboratory Medicine at UT Health McGovern Medical School and Biomedical Analytics, Houston, TX, USA:
“A 31-year-old white female was originally diagnosed with adrenocortical carcinoma (ACC) at age. She subsequently began chemotherapy that included doxorubicin, cisplatin, etoposide and mitotane and metyrapone at MD Anderson Cancer Center with some shrinkage of the tumor leading to its surgical removal via right adrenalectomy and right hepatectomy. However, her ACC returned a few months later with metastatic disease to the left side of her liver and left lower lobe of the lung, and the recurrent tumor was resistant to standard chemotherapy. When the patient was 26 years old, the metastatic tumor in the liver was excised via partial left hepatectomy and a portion was submitted for morphoproteomic analysis [8,9]. The morphoproteomic analysis resulted in the recommended therapeutic considerations that included a statin, metformin (500 mg twice per day) and melatonin (20 mg once per day at bedtime), and these agents were initiated as part of a personalized treatment plan of her medical oncologist. This brought the patient’s cancer under control clinically, and her improved health enabled her to start up her family. At age 27, the patient was pregnant, working part-time, and working out in the gym again. During her pregnancy and thereafter, she stopped the statin but continued metformin at 500 mg 4 times per week and melatonin at 20 mg 3 times per week as a maintenance regimen. She and her husband welcomed their daughter, born later that year. Subsequently, at age 28, a “spot” was confirmed in the right upper lobe of the lung and was removed and submitted for morphoproteomic analysis. By comparison with the pretreatment specimen from the liver, the metastatic tumor from the right upper lobe of the lung with the patient on maintenance therapy with metformin and melatonin showed molecular and morphometric evidence of growth inhibition (vide infra)."
"At age 29, repeat scans revealed no evidence of tumor, and she and her husband welcomed the birth of their son. Some 7 years post diagnosis the patient has resumed a healthy clinical life and remains on melatonin and metformin as a maintenance type therapy to reduce the risk of recurrent disease.”10. Green Tea (EGCG) and Cancer
However, the National Center for Complementary and Integrative Health (NCCIH) state that studies of green tea and cancer in humans have so far produced inconsistent results.
11. Mistletoe
Over 50 prospective studies (2020), including more than 30 randomized controlled trials (RCTs), have investigated the role of mistletoe in cancer patients, showing benefits in terms of improved quality of life, performance index, symptom scales, and reduced adverse effects of chemotherapy.12. Statins
Statins lower circulating blood lipids including low-density lipoprotein (LDL) cholesterol through the competitive inhibition of 3-hydroxy-3-methyl-glutaryl-coenzyme A reductase (HMGCR), an enzyme that facilitates the conversion of HMG-CoA to mevalonic acid, which is a crucial step in cholesterol biosynthesis. By inhibiting this process, statins not only reduce cholesterol production but also impact by-products essential for cancer cell growth, thereby demonstrating their potential as anticancer agents (source).13. The Gerson Therapy and Juicing
He was referring to Dr. Max Gerson, the German-born American medical doctor who developed one of the most effective natural cancer treatments about a century ago. Coined the “Gerson Therapy,” Dr. Gerson helped hundreds of cancer patients activate their bodies’ extraordinary ability to heal by recommending:
- Organic, plant-based foods
- Raw juices
- Coffee enemas
- Beef liver
- Natural supplements
In the words of the Gerson Institute:
With its whole-body approach to healing, the Gerson Therapy naturally reactivates your body’s magnificent ability to heal itself — with no damaging side effects. This a powerful, natural treatment boosts the body’s own immune system to heal cancer, arthritis, heart disease, allergies, and many other degenerative diseases.
How the Gerson Therapy Works
The Gerson Therapy targets the most significant metabolic requirements in your body. How? Believe it or not, this therapy allows you to reap the nutritional benefits of consuming 15–20 pounds of organically grown fruits and vegetables each day!
Here’s the breakdown:
- The Gerson Diet – Consisting of eating only organic fruits, vegetables and sprouted ancient grains, the Gerson Diet is exceptionally rich in vitamins, minerals and enzymes. It’s also very low in fats, proteins and sodium. The meal plan advises cancer patients to drink 13 glasses of freshly prepared juice, eat three plant-based meals and only snack on fresh fruits each day. Also, the traditional Gerson Therapy recommends consuming raw beef liver since it is the most nutrient-dense food on the planet and extremely high in vitamin B12.
- Juicing – According to the Gerson Institute, “Fresh pressed juice from raw foods provides the easiest and most effective way of providing high quality nutrition.” The cancer-fighting protocol calls for patients to drink fresh vegetables each day, including raw carrots or apples and green-leaf juice. To preserve the nutritional content, the juice should be prepared hourly using a two-step juicer or a masticating juicer used with a separate hydraulic press. This helps prevent denaturation — when vitamins, minerals and enzymes are destroyed. (Most commercial juicers spin so fast that they heat up juice to the point they are basically pasteurized!)
- Detoxification – The Gerson Therapy utilizes coffee enemas as the primary method of detoxing the body by increasing the parasympathetic nervous system. For cancer patients, this may take up to five enemas each day. The importance of keeping the body free of toxins is stressed by Dr. Gerson’s daughter, Charlotte:
The moment a patient is put on the full therapy, the combined effect of the food, the juices and the medication causes the immune system to attack and kill tumor tissue, besides working to flush out accumulated toxins from the body tissues. This great clearing-out procedure carries the risk of overburdening and poisoning the liver — the all-important organ of detoxification, which, in a cancer patient, is bound to be already damaged and debilitated.
- Supplements – The Gerson Therapy recommends the following organic medicinal therapies:
- Lugol’s solution
- Pancreatic enzymes
- Potassium compound
- Thyroid hormone
- Vitamin B12
14. Methylene Blue for Cancer
Methylene blue, a heterocyclic aromatic dye initially introduced as an antimalarial agent, has demonstrated various pharmacological activities, including antimicrobial, neuroprotective, and antioxidant properties. Recently, MB has emerged as a candidate for cancer therapy due to its ability to modulate oxidative stress and mitochondrial dynamics. This review consolidates current knowledge on MB's anticancer mechanisms and its translational potential in oncology.Recent research has provided further insights into MB's anticancer potential. A study by da Veiga Moreira et al. (2024) demonstrated that MB metabolic therapy effectively restrained in vivo ovarian tumor growth, suggesting its promise as a therapeutic approach for patients with platinum-resistant ovarian cancer.
Additionally, a systematic review by Lim (2023) supported the efficacy of MB-mediated photodynamic therapy against various cancer types, including colorectal tumors, carcinoma, and melanoma. These findings underscore the potential of MB in enhancing cancer treatment outcomes.
Furthermore, a study highlighted by Makis (2025) suggests that MB could be used as an adjunct to breast cancer surgery to eliminate microscopic residual malignant cells in the post-surgical cavity, potentially reducing recurrence rates.
"Our study indicated that MB and TMZ arrest GBM cells at different stages of the cell cycle; thus, an additive effect on GBM proliferation might be achievable with a combination therapy of MB and TMZ."
15. Stress Reduction, Sleep, and Sunshine
Mechanisms and Dosage:
- Sleep: Aim for 7-9 hours of restorative sleep each night.
- Stress Reduction Techniques: Practice meditation, deep breathing, or mindfulness exercises daily.
- Sunshine: Spend at least 15 minutes outdoors each day for natural vitamin D synthesis.
Considerations:
- If sleep disturbances are caused by cancer treatments, consult your healthcare provider for management strategies.
16. Berberine
Berberine is a plant compound with potential anticancer properties. It may inhibit cancer cell proliferation and induce apoptosis. Additionally, berberine has been shown to improve insulin sensitivity, which could be beneficial since high insulin levels are associated with certain cancers.Mechanisms and Dosage:
- Dosage: 500 mg two to three times daily.
- Mechanism: Activates AMPK pathway, inhibits tumor growth, and modulates the immune system.
🔍 Considerations:
- Blood glucose should be monitored and the additive/synergistic effect of metformin on the blood glucose profile should be determined.
- Berberine should not be taken in patients taking cyclosporine as this combination will increase cyclosporine levels (absolute contraindication).
- Berberine may alter the metabolism of the following drugs, which should be used with caution: anticoagulants, dextromethorphan, tacrolimus (Prograf), phenobarbitone, losartan (inhibits effect) and sedative drugs
👉 Did You Know? Berberine is featured in the FLCCC Insulin Resistance Protocol
17. Hyperthermia Therapy for Cancer
Hyperthermia is an abnormally high body temperature because your body can no longer release enough of its heat to maintain a normal temperature. It’s the opposite of hypothermia, when your body is too cold.
Hyperthermia vs Fever
A fever, on the other hand, is a temporary increase in your body temperature. Your hypothalamus increases your body’s set-point temperature often because your body’s attempt to fight off an infection.

Heat therapy for cancer
In addition, hyperthermia to treat cancer is also called thermal therapy, thermal ablation, or thermotherapy.
This application of heat also help enhance the efficiency of standard cancer therapies, such as chemotherapy and radiation treatment.
Hyperthermia in combined treatment of cancer:
Hyperthermia helps address the limitations of radiation for many patients by effectively increasing the radiation dose without increasing in unwanted side effects. (Source)
Hyperthermia and Radiotherapy in Metastatic Melanoma
A major multicenter trial was carried out in Europe by ESHO in patients with metastatic melanoma showed that here was a significant benefit for the addition of Hyperthermia, with a 2-year local control of 46% in the combined group as compared with 28% for those receiving Radiation alone. (Source)
b. Combination of Hyperthermia and Chemotherapy
Hyperthermia, with enhanced tissue perfusion, facilitates the absorption of chemotherapeutic API through cell membrane. In the presence of heat, chemical reaction gets accelerated. Therefore, chemotherapy becomes more effective, and less toxic. (Source)
18. HyperBaric Oxygen Therapy (HBOT) Chambers
~ Otto Warburg, MD (Nobel Prize in Physiology Winner, 1931)
Dr. Warburg made it clear that the root cause of cancer is oxygen deficiency, which creates an acidic state in the human body. He also discovered that cancer cells do not breathe oxygen and cannot survive in the presence of high levels of oxygen, as found in an alkaline state.
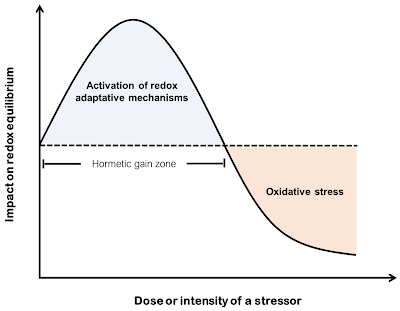
We’ve all heard that antioxidants help combat free radicals and reduce oxidative stress, which contributes to chronic disease. But is taking antioxidants alone enough to help treat cancer?
Probably not. That’s why incorporating oxygen therapy and using a hyperbaric chamber can be highly beneficial for those seeking natural cancer treatments.
19. DSMO and Cancer
- Inhibiting cancer growth: Laboratory studies suggest DMSO can slow the proliferation of various cancer cells, including bladder, breast, leukemia, prostate, ovarian, and lung cancers.
- Inducing apoptosis: DMSO may trigger programmed cell death in cancer cells, a key mechanism to control tumor growth.
- Enhancing chemotherapy: It can increase the absorption and effectiveness of chemotherapy drugs, potentially allowing lower doses and reducing side effects.
- Protecting healthy cells: DMSO may shield normal tissues from damage caused by radiation or chemotherapy.
- Stimulating immune response: By altering cancer cell properties, DMSO may make tumors more visible to the immune system.
20. BCG Treatment and Cancer
Conclusion
- Please do not consider this guide as personal medical advice, but as a recommendation for use by professional providers. Consult with your doctor and discuss with her/him.
- Our aim here isn't to replace your doctors' advice. It is intended as a sharing of knowledge and information. Do take note that cancer is a continuous struggle between the immune system and the cancer cells. Cancer treatments are meant to assist the immune system in this battle.
- Cancer treatment should be part of a multi-modal approach in order to provide the best possible outcome. Diet and lifestyle changes are meant to run alongside conventional treatment. They are complementary, not alternative.
- Cancer care is a team effort with the patient at the centre. Care should be supervised and coordinated by a primary healthcare provider. Patients with cancer should consult with their regular oncologist as well as an integrative provider/oncologist, in addition to their primary care provider and the supporting nurses, dieticians and other allied healthcare professionals.
- While the term 'alternative' might imply opposition to conventional oncology, we prefer 'complementary,' 'integrated,' or 'holistic.' These terms better reflect the role of these strategies as part of a personalized value-added menu of strategies, ensuring the most effective and safe solutions for patients.
- For an evidence-graded overview of repurposed cancer drugs, see our full guide.
Sources and References:
- Repurposed Drugs for Cancer (Townsend Letter)
- Drug repurposing for cancer therapy (Nature 2024)
- THE ROLE OF REPURPOSED DRUGS AND METABOLIC INTERVENTIONS IN TREATING CANCER (Independent Medical Alliance, previously known as FLCCC)
- Cancer Metabolism as a Therapeutic Target and Review of Interventions (Nutrients 2023)
- FLCCC Guide to Fasting and Healthy Eating
- Comprehensive overview of various cancers categorized by body system: https://cancer.aestheticsadvisor.com/p/cancer-types-by-system.html (Cancer Advisor 2025)
- Top 10 Metabolic Interventions & Repurposed Drugs for Cancer Treatment: 2025 Evidence-Based Review
- DMSO for Cancer (3 part series)
Find Integrative Oncologists in USA, Mexico, Europe or Asia
Consulting with an integrative healthcare expert is key to crafting a Fenbendazole protocol tailored to your unique health requirements.
New & Improved Joe Tippens Protocol
Below is a modified version of the Joe Tippens protocol, a synergistic combination of fenbendazole, ivermectin and nutraceuticals, updated based on the ivermectin and mebendazole based protocol published in the Journal of Orthomolecular Medicine (2024):
- Ivermectin (24 mg, 6 days a week) or in the case of severe aggressive cancers up to 1mg/kg/day.
- Mebendazole (Dose of 200 - 400 mg/day) or Fenbendazole, commonly taken at 300 mg for six days a week, with doses increasing to up to 1 gram in cases of aggressive cancers.
- Vitamin D (62.5 mcg [2500 IU] seven days a week).
- Bio-Available Curcumin (600 mg per day, 7 days a week).
- Enhanced absorption Berberine (500 mg per day) to starve your cancer of sugar.
- Diet and Lifestyle: Eliminate sugar consumption as supported by the BMJ 2023 umbrella review, which recommends reducing free and added sugars to below 25 g/day and limiting sugar-sweetened beverages to less than one serving per week to reduce adverse health effects. Adopt a whole-food diet and avoid ultra-processed foods, as recommended by the BMJ 2024 guidelines. Additionally, prioritise adequate sleep and effective stress management to support overall health.
- Please note that this protocol now includes the vital Vitamin D addition, with the one day off for the fenbendazole administration. This protocol represents the most comprehensive and cutting edge repurposed drug and vitamin treatment approach to date.
- If you are taking ivermectin and mebendazole, you might not need fenbendazole. Consult your doctor.
- Vitamin E: Removed from the protocol (Joe Tippens, July 22, 2020) due to interactions (e.g., with blood thinners).








.png)
.png)






Comments
Post a Comment