Higher Cholesterol Is Associated With Longer Life: Studies (2026)

|
| Buy on Amazon |
There are two types: High-density is the first. It is also known as HDL, or the “good” kind that keeps cholesterol away from your arteries and removes it from your arteries. The second type is low density lipoprotein, or LDL. LDL is the “bad” kind that can build up in your arteries, form plaque that narrows your arteries and form a clot. This can then make its way to your heart or brain and cause either a heart attack or stroke.
The American Heart Association (AHA) recommends that you balance your levels at about 150 (milligrams per deciliter) (mg/dL). According to old, unfounded science, your total cholesterol — the sum of all the cholesterol in your body — is not a gauge of your heart disease risk. When your levels are measured, elevated levels of triglycerides are also taken into account. According to Børge Nordestgaard, from the University of Copenhagen and Copenhagen University Hospital:
Does It Matter What Kills You?
In a commentary posted on Mission.org, a rhetorical question is presented: With all the ways you can die, does it really matter what kills you? On one hand, "If you're dead, you're dead, no matter from what," so it seems silly to "focus on changing something that lowers the risk of death from one cause only to raise that risk from another." (3)The Dietary Guidelines Advisory Committee (DGAC), which reviews the Dietary Guidelines for Americans every five years, investigated the issue. On page 91 of the 572-page report, the 2015-2020 guidelines noted: (5)
The 2015 DGAC will not bring forward this recommendation because available evidence shows no appreciable relationship between consumption of dietary cholesterol and serum (blood) cholesterol, consistent with the AHA/ACC (American Heart Association / American College of Cardiology) report. Cholesterol is not a nutrient of concern for overconsumption."
Yet, even though the government’s ChooseMyPlate doesn’t mention cholesterol, it’s obvious the cholesterol-is-evil myth is being pushed by physicians and medical agencies such as Harvard Health, which has proposed its own dietary guidelines called "The Healthy Eating Plate." (6)
Chastising the USDA for remaining "silent on fat," Harvard Health says this "could steer consumers toward the type of low-fat, high-carbohydrate diet that makes it harder to control weight and worsens blood cholesterol profiles."
It’s no wonder people are confused about where cholesterol fits in your diet, when major health agencies send one message to the public and the government sends a completely different one in their dietary guidelines.
Interestingly, the 2015-2020 guidelines were created nearly seven years ago, but information on the importance of cholesterol is nearly two decades old (7). As the Honolulu Heart Program study published in The Lancet in 2001 states:
The narrative challenges those who insist that eating foods that contain fat of any kind — saturated fats and trans fats alike — are harmful. Many who make this claim also maintain that "Saturated fat is a bad fat because it raises your LDL level more than anything else in your diet." (8)
Low Blood Cholesterol Associated with Increased Late Life Mortality?
Research published in Frontiers in Endocrinology (2024) found a revealing link between low total cholesterol (TC) levels and increased mortality risk in those aged 85 and above. This research challenges the conventional dogma that lower cholesterol is always better, especially for older adults.The study, which analyzed data from the Chinese Longitudinal Healthy Longevity Survey, found that individuals with TC (total cholesterol) levels below 3.40 mmol/L (131 mg/dL) had a significantly higher risk of all-cause mortality compared to those with higher levels.2 In fact, the mortality risk increased by 12% for every 1 mmol/L reduction in TC. These findings suggest that maintaining higher cholesterol levels may benefit longevity in your later years.
Study Challenges ‘Bad Cholesterol’ Label for LDL
Another 2024 study (JAMA) involving more than 4 million people across China challenges this belief, suggesting LDL may not be as harmful as previously thought—at least, not for everyone.Research led by Dr. Liang Chen and colleagues reveals a more nuanced picture. While high LDL levels are linked to increased mortality in some groups, they do not pose the same risk for others, they found. The relationship between LDL and mortality varies significantly based on an individual’s cardiovascular disease risk and overall health status.
Swedish Study Links High Cholesterol to Reaching 100
The 2023 AMORIS study in GeroScience tracked biomarkers from 44,636 Swedes aged 64-99, finding 1,224 who reached 100 showed higher total cholesterol and lower glucose compared to peers who died sooner. A popular post claims this proves high LDL cholesterol aids longevity and statins harm, urging low-carb diets with beef and eggs, but the study lacks LDL data and doesn't say every centenarian had high levels. Experts debate: some low-carb advocates see cholesterol as vital for health, while mainstream cardiology warns lifelong high LDL raises heart risks, proven by trials showing statins reduce deaths in high-risk patients.The Best Measure for Risk Factors
When it comes to your risk of death from heart disease, there’s much more evidence that inflammation is at the bottom of heart disease rather than high cholesterol, just as it is for a number of other serious diseases. If you want to find what might help you live longer, that’s the premise of a lengthy Japanese study published in the Annals of Nutrition & Metabolism (2015). As the featured study, it notes that regardless of someone’s age, people with higher cholesterol live longer:
Based on data from Japan, we propose a new direction in the use of cholesterol medications for global health promotion; namely, recognizing that cholesterol is a negative risk factor for all-cause mortality and re-examining our use of cholesterol medications accordingly."
After showing that people of all ages with higher cholesterol levels live longer in Japan, in support of these conclusions, similar conclusions were made by a study based in the Netherlands and published in BMJ in 2016. (11)
The study adjusted for several heart risk factors like smoking, high blood pressure and a history of diabetes melllitus. Participants were placed in groups depending on whether their cholesterol levels were low, medium or high, and those with the highest cholesterol levels were found to have the lowest death rates.
The title of the BMJ review reveals the outcome — there was a "lack of an association or an inverse association between low-density-lipoprotein cholesterol and mortality in the elderly."12
In short, older people with high LDL cholesterol generally live just as long as — and may even outlive — people with low LDL, which begs the question of how the current cholesterol theory was arrived at in the first place. At the very least, the study authors imply the cholesterol question should at least be re-evaluated. It concluded:
"Our review provides the basis for more research about the cause of atherosclerosis and (cardiovascular disease) and also for a re-evaluation of the guidelines for cardiovascular prevention, in particular because the benefits from statin treatment have been exaggerated."13One of the first studies published with information suggesting that high cholesterol is not as heart-damaging as once thought was the Honolulu Heart Program,14 offering further evidence that higher cholesterol levels may be heart protective. The authors concluded by questioning whether there is "scientific justification for attempts to lower cholesterol to concentrations below 4-65 mmol/L in elderly people," adding that "prudence dictates a more conservative approach in this age group."15
Can High Cholesterol Really Be Heart Protective?
- Cholesterol may protect against infections and atherosclerosis, as "the many observations that conflict with the LDL receptor hypothesis, may be explained by the idea that high serum cholesterol and/or high LDL is protective against infection and atherosclerosis."16
- Cholesterol may protect against cancer, although in previous cases where low cholesterol was linked to cancer, exclusions were made to tip the scales, such as excluding possible prior drug treatment, namely clofibrate, a popular cholesterol-lowering drug before statins, by subjects — leaving the question open as to whether it was the low cholesterol that caused the cancer, or the drug treatments that contributed to it.17
- Low cholesterol (180 mg/dL and lower) and violence in psychiatric patients have been linked. When patients in a long-term psychiatric hospital with a history of seclusion or restraints were compared with other patients, there was a "highly significant and strong association between lower cholesterol levels and violent behavior." The authors did caution, however, that cholesterol levels should not be used to predict violence.18
- There's also an association between low cholesterol and suicide dating back more than a decade, as researchers found that people in the lowest quartile of cholesterol concentration had more than six times the suicide rates than those in the highest quartile.19 It should be noted that at least one study in Japan20 determined that high cholesterol and suicide were connected. But, in fact, numerous recent studies have corroborated the earlier ones connecting low cholesterol to suicide,21 with various findings: For example, one found that low triglycerides, reduced BMI and waist circumference, specifically, but not total cholesterol, were connected to a higher risk of suicide;22 while a 2019 study23 found that "low cholesterol is associated with aggression in suicide attempters."
Cholesterol Could Boost Your Body’s Cancer-Fighting Abilities
Cholesterol Isn't the Problem in Heart Disease: Inflammation Is
The body tightly regulates the amount of cholesterol in the blood by controlling its production of cholesterol.
When your dietary intake of cholesterol goes down, your body makes more. When you eat greater amounts of cholesterol, your body makes less. Because of this, foods high in dietary cholesterol have very little impact on blood cholesterol levels in most people (R, R).
According to David Sinclair and Andrew Huberman, "Dietary cholesterol has zero impact on blood cholesterol levels."
Magnesium Plays Substantial Role in Reducing Inflammation
So What About Statins?
Significantly, the authors of an Annals of Nutrition & Metabolism study didn't hold back when drawing conclusions regarding why the cholesterol conundrum has gone on so long when the evidence is so clear: "For the side defending this so-called cholesterol theory, the amount of money at stake is too much to lose the fight."24
The Annals of Nutrition & Metabolism study's introduction mentions a medical practitioner who advocated statins to his patients to drive down cholesterol until he read the Scandinavian Simvastatin Survival Study,25 in which 4,444 patients with different types of heart disease were given simvastatin — which is touted to be a safe, long-term treatment to improve survival in cardiovascular heart disease patients.
As it turns out, the claim that high cholesterol causes heart disease and death is incorrect; it is, in fact, the opposite. Three reviews26,27,28 supporting the cholesterol hypothesis were found to contain altered data to support their conclusions, according to Expert Review of Clinical Pharmacology, in which it is noted that:
"Our search for falsifications of the cholesterol hypothesis confirms that … the conclusions of the authors of the three reviews are based on misleading statistics, exclusion of unsuccessful trials and by ignoring numerous contradictory observations."29Drugs.com30 contributors state that the 35 million people on statins often experience myriad side effects. Liver damage, for instance, is said to be "rare," implying that ongoing liver tests while taking statins likely aren't necessary. Some doctors, however, say you'll need a baseline liver function test beforehand. The most common side effects of statins are:
- Headaches, muscle pain, lower back or side pain
- Nasal congestion or stuffiness, or a runny nose
- Difficulty sleeping
- Constipation
- Hoarseness
And, just in case you needed another source to implicate statins' role in psychiatric problems, an April 2018 study found that lowering cholesterol levels in men could bring about changes in nerve cell membranes and behavior in men:
"Men seem to be more sensitive to low cholesterol levels as the association between low cholesterol levels and aggression is found mostly in men," the authors said. "… Lowering cholesterol levels with statins brings about several changes in the serotonergic system, nerve cell membrane microviscosity and behaviour, and needs to be done with precaution in susceptible individuals.Cholesterol levels could serve as a biological risk marker for violence and suicidal tendencies in psychiatric patients with depression and schizophrenia."
Statins aggravate insulin resistance through reduced blood GLP-1 levels in a microbiota-dependent manner
Statin Denial: An Internet-Driven Cult With Deadly Consequences?
If you find the recommendations of various professional groups confusing and prefer a well-rounded perspective, you’re in the right place.
In essence, there are two conflicting recommendations from doctors. We invite you to explore the evidence, sources, and references in this article and decide which perspective aligns best with your health priorities.
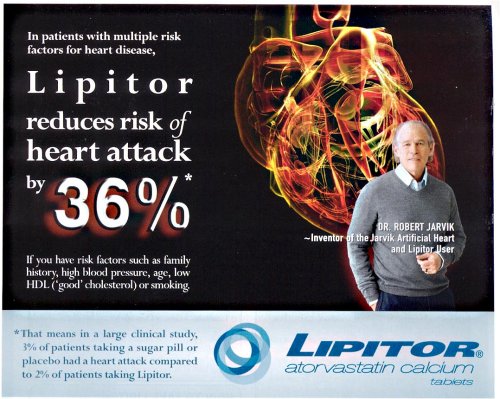
We also encourage you to consult with a trusted healthcare provider to discuss and weigh the benefits and risks of different treatment options.Reduces Risk of Heart Attack by 36%?
|
| Credit: Regenexx.com |
More Studies and Reviews on Statin Use
Rather than pointing patients in the direction of finding dietary solutions, including eating both the whites and the yolks when having eggs, and ditching processed vegetable oils in favor of healthy cooking oils like coconut oil, olive oil and avocado oil, Harvard Health Medical School updated an article on how to “manage” muscle pain from taking statins, perpetuating the cholesterol myth. They stated:
"If you're not taking a statin now, you may well be soon. These medications are commonly prescribed to lower 'bad' LDL cholesterol and have been shown to reduce the risk of heart attack, stroke, and death.They are routinely recommended for people who have cardiovascular disease and for many people ages 40 to 75 who don't have cardiovascular disease but have at least one risk factor (high blood pressure, high cholesterol, diabetes, or smoking) and a 7.5% or greater risk of a stroke or heart attack in the next decade.
Moreover, recent research indicates that they may benefit high risk individuals over age 75 as well … Taking a statin may give you some assurance that you're doing all you can to avoid heart attack and stroke …"31
Exercising, losing weight, adopting healthy eating habits and including vitamin D and coenzyme Q10 (CoQ10) supplements in your diet are all good strategies for maintaining your cholesterol levels. Unfortunately, the common suggestion for alleviating muscle pain due to statin use is more of the same — just try taking a lower dose or switching to another statin prescription.32
As if that weren't enough, experts say statins may impair your memory and cause amnesia, a possibility real enough to call for a warning on the labels of prescriptions.33 Statin use may precipitate a higher risk of developing cataracts34 and it "significantly" increases the likelihood of raising the fasting glucose levels of non-diabetics, as well as inducing high blood sugar.35
In another review of the adverse effects of statins, it was noted that "an array of additional risk factors for statin AEs [adverse events] are those that amplify (or reflect) mitochondrial or metabolic vulnerability, such as metabolic syndrome factors, thyroid disease, and genetic mutations linked to mitochondrial dysfunction."36
Given the false information saying cholesterol is at fault for causing heart-related disease, the continued prescriptions being handed out to patients for statins, and the side effects they cause, it's clear why, in their introduction, the authors of the Annals of Nutrition & Metabolism study stressed:37
"This, we believe, marks the starting point of a paradigm shift in not only how we understand the role cholesterol plays in health, but also how we provide cholesterol treatment …Our purpose in writing this supplementary issue is to help everyone understand the issue of cholesterol better than before, and we hope that we lay out the case for why a paradigm shift in cholesterol treatment is needed, and sooner rather than later."
Statin therapy is not warranted for a person with high LDL-cholesterol on a low-carbohydrate diet
Risk of Diabetes Doubles With Cholesterol Medication
Past studies have demonstrated that statins increase the risk of diabetes. Another study led by a graduate researcher at The Ohio State University explored this link in research published in Diabetes Metabolism Research and Reviews (2019). The study was a retrospective evaluation of medical records using employees and spouses from a private insurance plan.Yearly biometric screening, health surveys, medical claims and pharmacy data were gathered from 2011 through 2014. Individuals who had indications for statin use, or who had a previous cardiovascular event, were enrolled. Adults who had Type 2 diabetes before the study or who acquired it in the first 90 days were excluded.
Records were classified as belonging to a statin user if they had two or more prescriptions filled, but individuals using statins before January 2011 or within the first 90 days of enrollment in the insurance were excluded. Data were collected from 755 individuals using statins and 3,928 who were not.
After accounting for factors such as age, gender, ethnicity, education and body mass index, the researchers found those who used statins during the study were two times as likely to be diagnosed with diabetes than those who did not take statin medications.
Interestingly, individuals who used statin drugs longer than two years experienced an increased risk of more than three times as likely to get the disease. The data also indicated that individuals taking statin medications had a 6.5% increased risk of high blood sugar as measured by hemoglobin A1c values.
The hemoglobin A1c blood test is an average level of blood sugar measuring the past 60 to 90 days. The test measures how much sugar is bound to hemoglobin on red blood cells. Since red blood cells live for up to 90 days, the test is an average of your blood glucose level during this time.
Statins Increase Insulin Resistance
Statins have been shown to increase your risk of diabetes via a number of different mechanisms. The most important one is that they increase insulin resistance, which can be extremely harmful to your health. Secondly, statins increase your diabetes risk by raising your blood sugar. Statins work by preventing your liver from making cholesterol.As a result, your liver returns the sugar to your bloodstream, which raises your blood sugar levels. These drugs also rob your body of certain valuable nutrients, which can also impact your blood sugar levels. Two nutrients in particular, vitamin D and CoQ10, are both needed to maintain ideal blood glucose levels.
Importantly, statins deplete your body of CoQ10, vitamin K2, dolichol and selenium, thereby threatening your heart and overall health even further. Statins' ability to lower the risk of minor heart attacks may actually be related to their ability to lower C-reactive protein, far more so than the lowering of cholesterol.
Researchers with the Erasmus Medical Center in The Netherlands analyzed data from more than 9,500 patients. Those who had ever used statins had a 38% higher risk of Type 2 diabetes, with the risk being higher in those with impaired glucose homeostasis and those who were overweight or obese.
The researchers concluded, "Individuals using statins may be at higher risk for hyperglycemia, insulin resistance and eventually Type 2 diabetes. Rigorous preventive strategies such as glucose control and weight reduction in patients when initiating statin therapy might help minimizing the risk of diabetes."
But a far better strategy may be preventing insulin resistance in the first place, by avoiding statin drugs and eating a healthy diet. According to Malhotra and colleagues:
It is plausible that the small benefits of statins in the prevention of CVD come from pleiotropic effects which are independent of LDL-lowering. The focus in primary prevention should therefore be on foods and food groups that have a proven benefit in reducing hard endpoints and mortality."
CoQ10 and Statins
As a general rule, the sicker you are, the more you need. The suggested dose is usually between 30 mg to 100 mg per day if you're healthy, or 60 to 1,200 mg daily if you're sick or have underlying health conditions.
If you have an active lifestyle, exercise a lot or are under a lot of stress, you may want to increase your dose to 200 to 300 mg per day. Importantly, if you're on a statin drug, you need at least 100 mg to 200 mg of ubiquinol or CoQ10 per day, or more. Ideally, you'll want to work with your physician to determine your ideal dose.
Simple Strategies to Normalize Your Cholesterol Levels
Before becoming concerned about your cholesterol levels, it's important to evaluate whether you really need a statin drug to reduce your risk of a cardiovascular event. Updated guidelines published by the American Heart Association and the American College of Cardiology are based on a personalized risk assessment.However, the U.S. Department of Health and Human Services critically evaluates those with cholesterol levels over 200 milligrams per deciliter. We believe this total cholesterol measurement has little benefit in evaluating your risk for heart disease unless the number is over 300.
In some instances, high cholesterol may indicate a problem, provided it's your LDL or triglycerides and you have low HDL. A better evaluation of your risk of heart disease are these two ratios in combination with other lifestyle factors, such as your iron level and diet.
- HDL/Cholesterol ratio — Divide your HDL level by your cholesterol. This ratio should ideally be above 24%.
- Triglyceride/HDL ratio — Divide your triglyceride level by your HDL. This ratio should ideally be below 2. Data demonstrate a ratio greater than four is a powerful predictor of coronary artery disease.
Cholesterol for Healthy Immune Function
- Eat healthy fats: Focus on foods such as olive oil, avocado, fatty fish (such as salmon), and nuts, which provide good cholesterol and omega-3 fatty acids.
- Avoid trans fats: Processed snacks, baked goods, and fried foods can raise levels of “bad” cholesterol in your blood and lower the levels of “good” cholesterol.
- Exercise regularly: Physical activity helps regulate cholesterol and supports cardiovascular health, which is tied to a stronger immune system.
Make America Healthy Again
At the summit, he spoke about his vision of how to get America healthy, promoting a radical Scandinavian-style approach to health that would include raising the minimum wage, providing more affordable housing and improving educational outcomes.
“Modern medicine actually has relatively little role to play in terms of your health,” he says, arguing that “maybe 10 per cent of life expectancy or health is determined by what your doctor prescribes for you in the hospital or in the clinic”.
Instead, he says socially determined factors – the “conditions in which people are born, grow, live, work and age” – are the greatest contributors to overall health.
“If you are somebody who is in a low-pay, low-control, high-demand job, that, in a way, is effectively a death sentence in terms of the chronic stress it exerts,” he says.
- 1 AHA November 28, 2019
- 2 Medical News Today August 12, 2019
- 3, 9 Mission.org September 26, 2016
- 4 Neurology July 30, 2019
- 5 CNN. Cholesterol in Food Not a Concern, New Report Says. February 19, 2015
- 6 Harvard Health. Healthy Eating Plate vs. USDA’s MyPlate
- 7, 19 Epidemiology March 2001, Volume 12, Issue 2, pgs. 168-172
- 8 Medline Plus February 27, 2019
- 10, 24, 37 Annals of Nutrition & Metabolism April 30, 2015
- 11, 12, 13 BMJ June 12, 2016 Volume 6, Issue 6
- 14, 15 The Lancet August 4, 2001;358(9279):351-5
- 16 QJM: An International Journal of Medicine December 1, 2003
- 17 Q J Med 2012;105:383–388
- 18 Psychiatric Services February 1998;49(2):221-4
- 20 Acta Psychiatrica Scandanvica May 26, 2017 Volume 136 Issue 3
- 21 Annals of General Psychiatry April 17, 2017 Article number: 20 (2017)
- 22 Journal of Affective Disorders Volume 172, 1 February 2015, Pages 403-409
- 23 Psychiatry Research Volume 273 March 2019, Pages 430-434
- 25 The Lancet November 19, 1994; Volume 344, pgs. 1383-1389
- 26 The Lancet September 8, 2016; 388: 2532–61
- 27 JAMA September 27, 2016
- 28 European Heart Journal April 24, 2017; Volume 38, Issue 32, pgs. 2459–2472
- 29 Expert Review of Clinical Pharmacology October 11, 2018; Volume 11, Issue 10, pgs. 959-970
- 30 Drugs.com September 10, 2018
- 31 Harvard Health August 9, 2019
- 32 Medscape October 16, 2015
- 33 PLoS One September 10, 2013
- 34 JAMA November 2013
- 35 Cardiovascular Diabetology December 5, 2018
- 36 Am J Cardiovasc Drugs. April 6, 2008; 8(6):373-418
-
The Wellness Company's Base Spike Detox Trio
The first ever spike detox protocol appeared in the US Medical Literature and now it is available to you!
This base spike protein detox protocol consists of these three powerful ingredients: Spike Support's Nattokinase, Bromelain, and Tumeric Extract.
Vaccinated or not, prioritizing your well-being has never been more crucial.
Buy this ultimate detox bundle today, researched by Dr. Peter McCullough.
- Nattokinase and Bromelain are to be taken on an empty stomach, but Curcumin is with food.
- To get 10% OFF, please use this coupon code: ONEDAYMD
.png)
.png)

.png)






Comments
Post a Comment