Does Fenbendazole Raise Liver Enzymes? - Ben Fen
However, it is important to interpret these findings within the context of cancer therapy as a whole. Temporary elevations in AST and ALT can occur as the liver processes cellular debris resulting from cancer cell death induced by an effective treatment like fenbendazole. This hepatic stress may reflect increased workload rather than necessarily indicating intrinsic drug toxicity.
Such fluctuations are commonly observed during recovery from various illnesses involving significant cell turnover and often normalize after the underlying condition, such as cancer burden, resolves. Therefore, transient liver enzyme elevations during fenbendazole therapy may, in some contexts, signify effective tumor lysis rather than adverse drug-induced liver injury. As such, liver enzyme values should be monitored, as they would be during most cancer therapies, for changes and to determine the nature of those changes, that is, either transient or longer-term.
Liver Enzymes, Fenbendazole and Cancer
We examined our Case Reports and in some instances, ALT and AST rose during treatment with fenbendazole. The elevation was phasic and resolved to levels within normal limits within three or four months. While these observations could reflect primary hepatic disruption by fenbendazole, it is highly unlikely for several reasons. First, not all case reports detected alterations in AST or ALT. Second, all instances were temporary and resolved in short order. Third, the return to normalcy was maintained despite continued administration of fenbendazole.
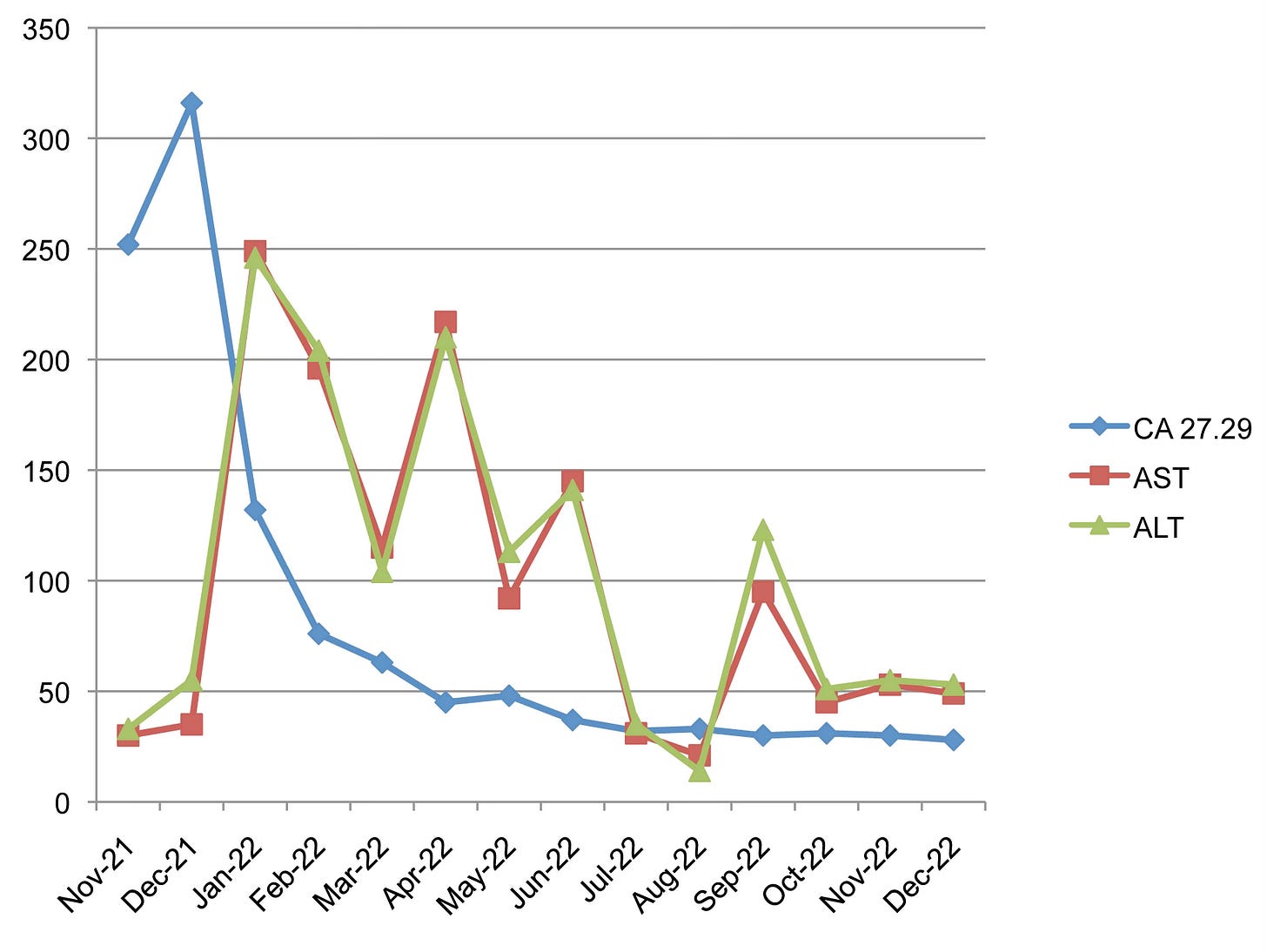
As an example, the figure above is for an 83 yr old with metastatic breast cancer who started self-treating with fenbendazole in December of 2021. Plotted are AST and AST liver enzyme measurements and blood tumor marker CA 27.29 values from initial diagnosis through the subsequent year. If we take a look at the figure above what is very interesting is the time course of the AST/ALT elevations. Initially before fenbendazole treatment AST/ALT were within normal limits (the green and orange markers) and then peaked as the blood tumor cancer marker CA 27.29 (blue marker) started to drop precipitously. Presumably this drop in blood tumor marker reflected the eradication of the cancer, which it did as verified by concurrent CT and PET imaging.
It certainly appeared that the transient elevations in liver enzymes coincided with the active phase of fenbendazole anticancer activity. That is, elevations of AST and ALT, which are broadly accepted as indices of liver stress and/or the stress associated with increased workloads as would be expected with massive die-offs of malignant cells. Once the bulk of the die-off was over (Dec 21 to Feb 22), the cancer is eradicated as evidenced by the flattening of the blue line to within normal limits, there is less dead cancer cell debris to clear through the liver and the liver enzymes return to baseline. It is important to note that she continued to take fenbendazole daily throughout this period (and still does). Maintenance of this liver status quo regarding normal enzymes persists despite continued fenbendazole administration.
What are the takeaways regarding liver enzyme dynamics, fenbendazole, and cancer?
First, fenbendazole, in the dose used here (222 mg and 444 mg), is not a hepatotoxin, consistent with what has been demonstrated over billions of doses, over the more than sixty years of antiparasitic use of fenbendazole, mebendazole and albendazole.
Second, the transient rise in AST and ALT may reflect a Herxheimer-type reaction due to the die-off of massive amounts of malignant cells.
Third, the return to baseline values of liver function appears to reflect the clearing of the dead cancer cellular debris because these liver values return to within normal limits despite the continued use of fenbendazole. That is, if fenbendazole was the direct cause of liver stress, AST/ALT values would remain elevated as long as fenbendazole was present. She continues to take fenbendazole during the immediate post-remission period as well as indefinitely afterward. Subsequently, liver enzymes are measured regularly with standard blood panels, and they are normal.
In summary, the likely process that is being observed in the figure above is that fenbendazole results in a massive die-off of cancer cells, causing a temporary hepato-stressor event reflected in transient AST/ALT rise; once the cancer is cleared, this stress on the liver declines, as does AST/ALT. As such, the transient rise in ALT/AST in some cases may serve as a gauge of the effectiveness of fenbendazole in killing a specific cancer. This observation may create a wealth of opportunity regarding further study of the factors that may affect the magnitude, specificity, time course, effectiveness, and persistence of the fenbendazole anticancer effect using AST/ALT values as a marker.
This is not to say that this mechanism is the only possibility, or that it will occur in all situations. To identify and understand how fenbendazole and other anti-parasitic drugs being used for cancer treatment interact with other drugs and idiosyncratic physiological states awaits future targeted research.
To Better Understand Some of the Issues Involved Here is Some Background Information on Drug Effects on Liver Function
Mechanisms of Liver Enzyme Elevation
Elevated AST and ALT are not specific for drug toxicity alone. They may increase for several reasons, including:
Tumor lysis syndrome: Rapid destruction of cancer cells can overwhelm hepatic clearance pathways, resulting in transient enzyme elevation as the liver metabolizes cellular breakdown products.
General cell turnover: Similar enzyme spikes are seen with immune therapies, radiation, or other cytotoxic agents where effective antitumor response causes hepatocyte stress but not necessarily direct damage.
Non-specific hepatic workload: Recovery from serious illness or other treatments can transiently tax hepatic function, with enzyme normalization occurring after resolution.
Liver enzymes may increase during many noncancerous conditions involving increased cell turnover, muscle injury, strenuous exercise, hemolysis, and tissue repair, as enzymes such as AST and ALT are also present in tissues beyond the liver. During illness or recovery, these transient elevations reflect the liver clearing dead or damaged cells and are considered part of normal physiological processes. Most such elevations are temporary and normalize upon recovery of the underlying disease or after metabolic debris has been cleared.
Malakouti M, Kataria A, Ali SK, Schenker S. Elevated Liver Enzymes in Asymptomatic Patients – What Should I Do?J Clin Transl Hepatol. 2017;5(4):394-403. doi: 10.14218/JCTH.2017.00027.
Giannini, E. G., Testa, R., & Savarino, V. (2005). Liver enzyme alteration: a guide for clinicians. CMAJ : Canadian Medical Association Journal, 172(3), 367–379. https://doi.org/10.1503/cmaj.1040752
The process of dead cell clearance by the liver and tissue macrophages (efferocytosis) is a well-characterized mechanism that helps resolve inflammation and support tissue regeneration. This involves hepatocytes and phagocytic cells engulfing cellular debris, which may transiently stress liver function and lead to measurable but non-pathological fluctuations in liver enzymes.
Boada-Romero, E., Martinez, J., Heckmann, B. L., & Green, D. R. (2020). The clearance of dead cells by efferocytosis. Nature Reviews. Molecular Cell Biology, 21(7), 398–414. https://doi.org/10.1038/s41580-020-0232-1
Research Specific to Fenbendazole and Cancer Cell Death
Fenbendazole is demonstrated in recent studies to induce apoptosis and pyroptosis in cancer cells, leading to rapid cell death and the release of cellular breakdown products. As these products are transported to the liver for processing and elimination, a predictable but temporary rise in AST and ALT is observed, paralleling the physiological processes seen in other conditions involving high rates of cell turnover.
Pan, C. et al. Fenbendazole induces pyroptosis in breast cancer cells through HK2/caspase-3/GSDME signaling pathway. Frontiers in Pharmacology, 17 July 2025, Sec. Pharmacology of Anti-Cancer Drugs.Volume 16 - 2025 | https://doi.org/10.3389/fphar.2025.1596694
Temporary and moderate elevations in liver enzymes are recognized in the literature during effective cancer treatments, including those involving fenbendazole, and should be monitored as a matter of course. Such changes may not reflect direct hepatotoxicity but rather increased hepatic workload due to the therapy’s anticancer actions.
Biggers, A. (2025). Can Liver Enzyme Levels Fluctuate? https://www.healthline.com/health/can-liver-enzymes-fluctuate#fluctuation-causes
General Liver Enzyme Fluctuation
Medical sources confirm that elevated liver enzymes can result from a wide spectrum of benign, transient, and reversible causes—including recovery from illness, infection, or inflammation, or after intense physical exertion—and that normalization is expected as the triggering process resolves.
Aizawa, S., Brar, G., & Tsukamoto, H. (2020). Cell Death and Liver Disease. Gut and Liver, 14(1), 20–29. https://doi.org/10.5009/gnl18486
Transient increases in AST/ALT may indeed reflect therapy-induced cell death, especially if no other signs of liver dysfunction (e.g., jaundice, coagulopathy) are present. This pattern is recognized during the course of many anticancer agents, where clinicians expect, monitor, and distinguish between benign and pathologic enzyme changes. Persistent or worsening elevations, especially combined with other abnormal labs, would warrant investigation for genuine drug induced injury.
Since acetaminophen (Tylenol) is in the news we thought it useful to see what was known about it in relation to fenbendazole. It is very important to never co-administer acetaminophen with fenbendazole. Acetaminophen is often present in cold, flu, allergy and pain medications, read the labels. It is essential to never combine the two as a mouse study found that very high dose fenbendazole (equivalent to 1200 mg per day for a human) appears to interact in unknown ways to increase the liver hepatotoxic effects of acetaminophen. What was interesting is that high dose of fenbendazole did not affect any measure of liver function by itself. It was only when combined with high dose acetaminophen that liver function was affected. Acetaminophen is toxic to the liver, avoid it
Source: Gardner, C. R., Mishin, V., Laskin, J. D., & Laskin, D. L. (2012). Exacerbation of acetaminophen hepatotoxicity by the anthelmentic drug fenbendazole. Toxicological Sciences, 125(2), 607–612. https://doi.org/10.1093/toxsci/kfr301Conclusion
Interpreting transient liver enzyme rises during fenbendazole or cancer therapy requires context: such changes are not uncommon in intensive cancer treatment and, if temporary, may signal successful tumor death rather than drug harm. Continuous monitoring is essential to distinguish benign from harmful patterns.
The elevated liver enzymes may actually a good sign for a cancer patient taking fenbendazole. Those liver enzyme (AST, ALT) values may spike for several months as the liver is processing the flood of dead cancer cells as it filters and processes the cellular debris from the dead cancer cells. AST and ALT increasing is a sign of hepatic stress (work) not necessarily disease in the context of fenbendazole use. These liver enzymes appear to normalize after the cancer is eradicated by fenbendazole.
As a side note to the Yamaguchi et al. (2021) study there was a serious confounding factor present in that report: the woman was also taking the PD-L1 immunotherapy drug (pembrolizumab [Keytruda]) that does list hepatic damage as a major side effect. She was on Keytruda ineffectually for many months before trying fenbendazole for one month as a last resort, at which time her liver function markers changed. It is unknown whether the accumulated effects of the immunotherapy drug caused the liver changes, an interaction between fenbendazole and the pembrolizumab occurred, and/or the lysis phenomenon described above occurred, signaling fenbendazole effectiveness in eradicating her cancer.
Source: Calderon, B., Stancu, A., Vanel, F. R., & Vazquez, L. (2021). Pembrolizumab Treatment-Induced Liver Toxicity. Case Reports in Gastroenterology, 15(2), 742–750. https://doi.org/10.1159/000518128- Cray, C., & Altman, N. H. (2022). An Update on the Biologic Effects of Fenbendazole. Comparative Medicine, 72(4), 215–219. https://doi.org/10.30802/AALAS-CM-22-000006
- Gardner, C. R., Mishin, V., Laskin, J. D., & Laskin, D. L. (2012). Exacerbation of acetaminophen hepatotoxicity by the anthelmentic drug fenbendazole. Toxicological Sciences : an official journal of the Society of Toxicology, 125(2), 607–612. https://doi.org/10.1093/toxsci/kfr301
- Yamaguchi, T., Shimizu, J., Oya, Y., Horio, Y., & Hida, T. (2021). Drug-induced liver injury in a patient with nonsmall cell lung cancer after the self-administration of fenbendazole based on social media information. Case Reports in Oncology 14, no. 2: 886–91. doi.org/10.1159/000516276
.png)

.png)



.png)


Comments
Post a Comment