Omicron September 2022: How to Treat Omicron Symptoms
As of the week ending September 17, 2022, BA.5 represent an estimated 84.8% of the SARS-CoV-2 variants currently circulating in the United States, according to the CDC. The BA.4.6 Omicron subvariant is the second most prevalent with 10.3% of cases originating from the pathogen.
BA.5 is one of many Covid-19 Omicron subvariants to emerge since last winter. The subvariant is also driving up cases in parts of Europe and North America and has become the dominant U.S. Omicron strain. This version of the virus is believed to spread particularly easily, fueled in part by its ability to evade immunity built up from vaccines and prior infections.
The range of possible symptoms is wide but centers on the upper respiratory system.
According to the US CDC (updated August 2022), people with COVID-19 have had a wide range of symptoms reported – ranging from mild symptoms to severe illness. Symptoms may appear 2-14 days after exposure to the virus. Anyone can have mild to severe symptoms.
Possible symptoms include:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
Because these symptoms can easily be mistaken for a common cold, especially during a time when travel restrictions are being lifted, many choose not to seek out a COVID-19 test initially — until other symptoms present later down the road.
That said, there are two specific symptoms that could be signs that a positive COVID-19 test is coming, according to The Independent:
- Fatigue.
- Spells of dizziness or fainting.
Take a Test
Between 48 and 72 hours after potential COVID exposure or at the first sign of any symptoms, people should take either a rapid antigen or PCR test. “There should be a very low threshold for testing yourself to see whether you have COVID or whether you have something else,” says Amesh Adalja, a senior scholar at the Johns Hopkins Center for Health Security. COVID can look very like a cold, influenza or allergies, but the treatments for each are different.
PCR tests are more sensitive but harder to get, and taking a rapid antigen test at home usually suffices, the experts say. If the first test is negative, people should wait two days (behaving cautiously in the meantime) and take another one as Myers did. If it is COVID, the viral load will increase in that time. “Nothing in life is perfect, nor are the rapid antigen tests, but they’re pretty darn good at picking up contagious levels of virus,” says Lucy McBride, a practicing primary care doctor in Washington, D.C. (Lists of free test locations are available on the Test to Treat locator Web site provided by the U.S. Department of Health and Human Services.)
When people test positive, it is a good idea for them to call a primary care physician if they have one. Doctors can provide guidance on treatment and update medical histories. They will also report the result to public health authorities so that it is included in case counts. At a minimum, people should track the date that symptoms began and the date of a positive test.
Between 48 and 72 hours after potential COVID exposure or at the first sign of any symptoms, people should take either a rapid antigen or PCR test. “There should be a very low threshold for testing yourself to see whether you have COVID or whether you have something else,” says Amesh Adalja, a senior scholar at the Johns Hopkins Center for Health Security. COVID can look very like a cold, influenza or allergies, but the treatments for each are different.
PCR tests are more sensitive but harder to get, and taking a rapid antigen test at home usually suffices, the experts say. If the first test is negative, people should wait two days (behaving cautiously in the meantime) and take another one as Myers did. If it is COVID, the viral load will increase in that time. “Nothing in life is perfect, nor are the rapid antigen tests, but they’re pretty darn good at picking up contagious levels of virus,” says Lucy McBride, a practicing primary care doctor in Washington, D.C. (Lists of free test locations are available on the Test to Treat locator Web site provided by the U.S. Department of Health and Human Services.)
When people test positive, it is a good idea for them to call a primary care physician if they have one. Doctors can provide guidance on treatment and update medical histories. They will also report the result to public health authorities so that it is included in case counts. At a minimum, people should track the date that symptoms began and the date of a positive test.
Over-the-Counter Help
Most people who get COVID will be just fine at home. “If you’re vaccinated and boosted and generally healthy, people do very well,” McBride says. Over-the-counter medications will not treat COVID directly but can help manage symptoms. Doctors recommend acetaminophen (Tylenol) or non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil or Motrin) to bring down fevers and relieve achiness. Early in the pandemic, there were reports that ibuprofen made COVID worse, but those have not been substantiated. NSAIDs are only intended to be taken for short periods, however, because they have more side effects than acetaminophen, and they are not safe for everyone. People who take other medications should consult with a doctor before taking NSAIDs. Antihistamines or cold medications such as DayQuil can be used to relieve congestion and cough.
All over-the-counter medications should be taken as needed and not beyond recommended dosage instructions (some cold medicines already include acetaminophen). “The dose and frequency really depend on the patient’s underlying health conditions and should be discussed with the person’s doctor,” McBride says.
Most people who get COVID will be just fine at home. “If you’re vaccinated and boosted and generally healthy, people do very well,” McBride says. Over-the-counter medications will not treat COVID directly but can help manage symptoms. Doctors recommend acetaminophen (Tylenol) or non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil or Motrin) to bring down fevers and relieve achiness. Early in the pandemic, there were reports that ibuprofen made COVID worse, but those have not been substantiated. NSAIDs are only intended to be taken for short periods, however, because they have more side effects than acetaminophen, and they are not safe for everyone. People who take other medications should consult with a doctor before taking NSAIDs. Antihistamines or cold medications such as DayQuil can be used to relieve congestion and cough.
All over-the-counter medications should be taken as needed and not beyond recommended dosage instructions (some cold medicines already include acetaminophen). “The dose and frequency really depend on the patient’s underlying health conditions and should be discussed with the person’s doctor,” McBride says.
Getting enough rest is critical, as is drinking enough fluids, which prevent dehydration and reduce cough.
Having a pulse oximeter at home would also be useful to calculate the amount of oxygen in a person’s blood without having to draw a blood sample. If oxygen levels fall below 95 per cent, that would be a sign to visit the hospital.
Thermometers, tissues and hand sanitizer are other supplies often recommended to keep at home while experiencing a COVID-19 infection. Finally, it won’t hurt to take vitamin supplements (read details below).
Using Prescription Drugs
One of the most significant recent changes in the COVID landscape is the wider availability of authorized outpatient treatments. The antiviral drug Paxlovid reduced risk of hospitalization and death by 89 percent in a clinical trial, and it is a pill, which makes it relatively easy to take. The drug cannot be taken with many common medications such as statins or blood thinners, however. Monoclonal antibodies also significantly reduce the risk of severe disease, but they require an injection or infusion. And not every patient is eligible to get these treatments. Both have been authorized for people who are at higher risk of severe illness because of age (65 and older) or underlying health conditions such as high blood pressure or lung disease. To date, there is no evidence that these treatments benefit people who are young or otherwise healthy. Either treatment is available by prescription or at Test to Treat sites nationwide for people who are eligible.
To be effective, these medications must be started soon after symptoms begin (within five days and seven days, respectively). “[People who might be eligible] should call their provider right away,” says Raymund Razonable, an infectious disease specialist at the Mayo Clinic. “These treatments work best when the patients are not feeling so bad.” Side effects of Paxlovid are uncommon but include diarrhea and a metallic taste in the mouth.
One of the most significant recent changes in the COVID landscape is the wider availability of authorized outpatient treatments. The antiviral drug Paxlovid reduced risk of hospitalization and death by 89 percent in a clinical trial, and it is a pill, which makes it relatively easy to take. The drug cannot be taken with many common medications such as statins or blood thinners, however. Monoclonal antibodies also significantly reduce the risk of severe disease, but they require an injection or infusion. And not every patient is eligible to get these treatments. Both have been authorized for people who are at higher risk of severe illness because of age (65 and older) or underlying health conditions such as high blood pressure or lung disease. To date, there is no evidence that these treatments benefit people who are young or otherwise healthy. Either treatment is available by prescription or at Test to Treat sites nationwide for people who are eligible.
To be effective, these medications must be started soon after symptoms begin (within five days and seven days, respectively). “[People who might be eligible] should call their provider right away,” says Raymund Razonable, an infectious disease specialist at the Mayo Clinic. “These treatments work best when the patients are not feeling so bad.” Side effects of Paxlovid are uncommon but include diarrhea and a metallic taste in the mouth.
Based on a lab study (NEJM, July 2022) using the live-virus Focus Reduction Neutralization Testing (FRNT) method, bebtelovimab seems to be the most promising monoclonal antibody against the BA 5 subvariant.
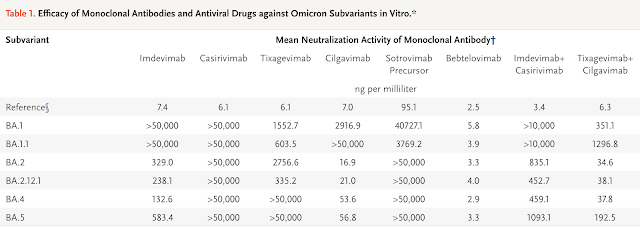
Overall, the study data also suggest that the three antiviral drugs remdesivir, molnupiravir, and nirmatrelvir (Paxlovid) may still have therapeutic value against the sublineages BA.2.12.1, BA.4, and BA.5 of SARS-CoV-2 omicron variants.

Do take note of the limitation of this study as this is a non-clinical study (not in humans). There is lack of clinical data on the efficacy of these monoclonal antibodies and antiviral drugs for the treatment of patients infected with BA.4 or BA.5 subvariants. Therefore, the selection of monoclonal antibodies or anti-virals to treat patients who are infected should be carefully considered based on the potential risks as compared to its potential benefits.
In India and Nepal, the prevalence of a subvariant of BA.2 (designated BA.2.75) is increasing rapidly and is now becoming dominant in Nepal (R). Moreover, BA.2.75 has been detected in at least 25 other countries, including the United States, Singapore, Canada, the United Kingdom, Japan, and Australia; as such, it has spread across multiple continents (R). The World Health Organization designated BA.2.75 as a “variant of concern lineage under monitoring.”
Based on a lab study (NEJM, September 2022) using the live-virus Focus Reduction Neutralization Testing (FRNT) method, bebtelovimab seems to be the most promising monoclonal antibody against the BA 2.75 subvariant.
REGN10987 (marketed as imdevimab) lost neutralizing activity against BA.2.75, whereas REGN10933 (marketed as casirivimab) retained some neutralizing activity against the isolate. REGN10987 in combination with REGN10933 (casirivimab–imdevimab) inhibited BA.2.75; however, the neutralizing activity against BA.2.75 with this combination was less than that against the ancestral strain (SARS-CoV-2/UT-NC002-1T/Human/2020/Tokyo) by a factor of 812.5.
COV2-2196 (marketed as tixagevimab) and COV2-2130 (marketed as cilgavimab) neutralized BA.2.75. The COV2-2196 plus COV2-2130 combination (tixagevimab–cilgavimab) inhibited BA.2.75 with a low FRNT50 value (34.19 ng per milliliter), but the neutralizing activity was less than that against the ancestral strain by a factor of 5.3. The precursor of sotrovimab (S309) neutralized BA.2.75 weakly; however, its activity was less than that against the ancestral strain by a factor of 870.0.
Of the monoclonal antibodies tested, only LY-CoV1404 (marketed as bebtelovimab) efficiently neutralized BA.2.75 (FRNT50 value, 6.21 ng per milliliter).
Overall, the study data also suggest that the three antiviral drugs remdesivir, molnupiravir, and nirmatrelvir may still have therapeutic value against the BA 2.75 of SARS-CoV-2 omicron variant.
Other At-Home Treatments
You can find a listing of doctors who can prescribe necessary home isolation medications on Find a Provider post.
There are many COVID-19 treatment protocols out there on the internet. We have reviewed many protocols and believe the FLCCC I-CARE protocol is one of the easiest and effective protocols to follow.
Based on recent clinical experience treating Omicron patients, the Front Line COVID-19 Critical Care Alliance (FLCCC) modified its early treatment protocol to include hydroxychloroquine as "preferred for Omicron".
The Omicron variant of the SARS-CoV-2 virus apparently enters human cells differently than do other variants. Analysis of biological mechanisms for hydroxychloroquine indicate that it has enhanced efficacy for the early treatment of Omicron, especially when coupled with zinc.
The Front Line COVID-19 Critical Care Working Group (FLCCC) recommends hydroxychloroquine and ivermectin as part of their I-CARE protocol for early outpatient treatment of COVID-19 (June 29, 2022 version).
The Omicron variant of the SARS-CoV-2 virus apparently enters human cells differently than do other variants. Analysis of biological mechanisms for hydroxychloroquine indicate that it has enhanced efficacy for the early treatment of Omicron, especially when coupled with zinc.
Specifically, they recommend hydroxychloroquine (preferred for Omicron) and ivermectin as first line anti-viral agents:
- Ivermectin: 0.4–0.6 mg/kg per dose (take with or after meals) — one dose daily, take for 5 days or until recovered. (Find a Doctor). Use upper dose range if: 1) in regions with more aggressive variants (e.g. Delta); 2) treatment started on or after day 5 of symptoms or in pulmonary phase; or 3) multiple comorbidities/risk factors. (Ref)
- Hydroxychloroquine (preferred for Omicron): 200mg PO twice daily; take for 5 days or until recovered. (Find a Doctor)
Always consult your trusted medical professional before you take any medication or supplement.
Long COVID risk less from omicron variant than from delta
The omicron variant is less likely to cause long COVID than the delta variant, new research has found. Analysis by researchers from King's College London of data from the ZOE COVID Symptom study app is published in The Lancet (June 2022). The findings are from the first peer-reviewed study to report on long COVID risk and the omicron variant.
Long COVID is defined by NICE guidelines as producing new or ongoing symptoms four weeks or more after the start of disease. Symptoms include fatigue, shortness of breath, loss of concentration and joint pain. The symptoms can adversely affect day-to-day activities, and in some cases can be severely limiting. Researchers found the odds of experiencing long COVID were between 20-50% less during the omicron period versus the delta period, depending on age and time since vaccination.
The UK Office of National Statistics estimated the numbers of people with long COVID actually increased from 1.3 million in January 2022 to 2 million as of May 1, 2022.
Lead author, Dr. Claire Steves from King's College London, said, "The omicron variant appears substantially less likely to cause long COVID than previous variants, but still 1 in 23 people who catch COVID-19 go on to have symptoms for more than four weeks.
Emergency warning signs
Individuals are reminded to seek immediate medical attention (go to a hospital’s emergency department) if they develop emergency warning signs of COVID-19 such as:
- Difficulty breathing
- Persistent pain or pressure in the chest
- Bluish lips or face
- New confusion or inability to arouse
Key Takeaway
As soon as you have symptoms, consult your healthcare provider and start treatment as early as possible. If treatment is delayed i.e. after 5 days of symptoms, your chances of severe COVID are higher.



.png)
.png)






Comments
Post a Comment