Optimizing Vitamin D RDAs: A Key Public Health Initiative for MAHA (2025)
The Big Vitamin D Mistake
Since 2006, type 1 diabetes in Finland has plateaued and then decreased after the authorities’ decision to fortify dietary milk products with cholecalciferol. The role of vitamin D in innate and adaptive immunity is critical. A statistical error in the estimation of the recommended dietary allowance (RDA) for vitamin D was recently discovered; in a correct analysis of the data used by the Institute of Medicine, it was found that 8895 IU/d was needed for 97.5% of individuals to achieve values ≥50 nmol/L. Another study confirmed that 6201 IU/d was needed to achieve 75 nmol/L and 9122 IU/d was needed to reach 100 nmol/L. The largest meta-analysis ever conducted of studies published between 1966 and 2013 showed that 25-hydroxyvitamin D levels <75 nmol/L may be too low for safety and associated with higher all-cause mortality, demolishing the previously presumed U-shape curve of mortality associated with vitamin D levels. Since all-disease mortality is reduced to 1.0 with serum vitamin D levels ≥100 nmol/L, we call public health authorities to consider designating as the RDA at least three-fourths of the levels proposed by the Endocrine Society Expert Committee as safe upper tolerable daily intake doses. This could lead to a recommendation of 1000 IU for children <1 year on enriched formula and 1500 IU for breastfed children older than 6 months, 3000 IU for children >1 year of age, and around 8000 IU for young adults and thereafter. Actions are urgently needed to protect the global population from vitamin D deficiency.
Statistical Error in Vitamin D RDA
The statistical error in the estimation of the Recommended Dietary Allowance (RDA) for vitamin D occurred because the Institute of Medicine (IOM) misinterpreted its own statistical analysis. The IOM estimated that 600 IU/day of vitamin D would ensure that 97.5% of individuals reach a serum 25-hydroxyvitamin D (25(OH)D) level of 50 nmol/L. However, their calculation was incorrect because they mistook the lower prediction limit for individuals as the lower limit for group averages.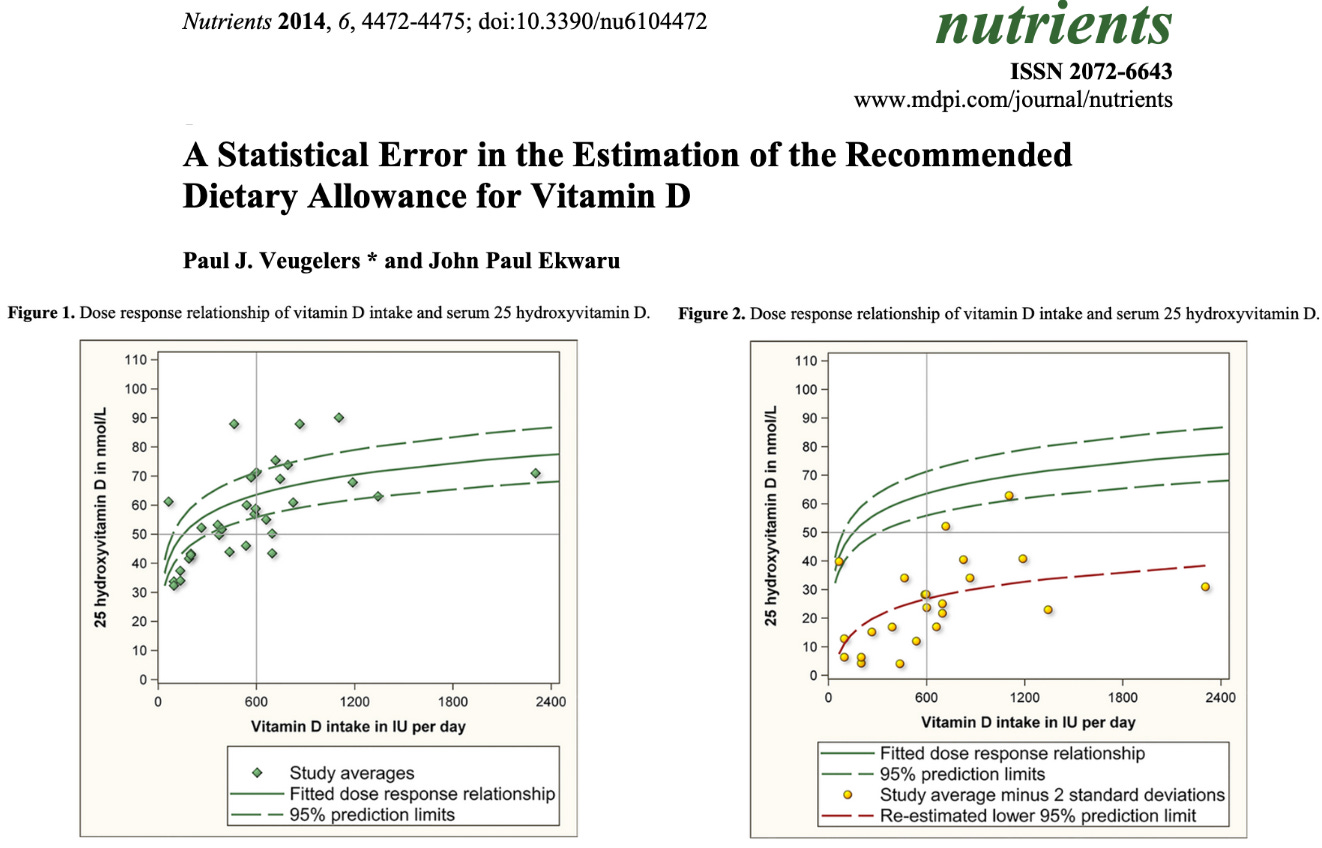
Vitamin D Dosage Recommendations
In the US, current guidelines suggest that consuming 400–800 IU (10–20 mcg) of vitamin D should meet the needs of 97–98% of all healthy people (Source).However, many experts believe the guidelines are far too low (Source).
Your vitamin D needs depend on a variety of factors. These include your age, skin color, current blood vitamin D levels, location, sun exposure and more.
To reach blood levels linked to better health outcomes, many studies have shown that you need to consume more vitamin D than the guidelines recommend (Source, Source, Source).
For instance, an analysis of five studies examined the link between vitamin D blood levels and colorectal cancer (Source).
Scientists found that people with the highest blood levels of vitamin D (over 33 ng/ml or 82.4 nmol/l) had a 50% lower risk of colorectal cancer than people with the lowest levels of vitamin D (less than 12 ng/ml or 30 nmol/l).
Research also shows that consuming 1,000 IU (25 mcg) daily would help 50% of people reach a vitamin D blood level of 33 ng/ml (82.4 nmol/l). Consuming 2,000 IU (50 mcg) daily would help nearly everyone reach a blood level of 33 ng/ml (82.4 nmol/l) (Source, Source, Source).
- Deficiency: Less than 20 ng/ml (50 nmol/L)
- Insufficiency: 21 - 29 ng/ml (52 - 72 nmol/L)
- Sufficiency: More than 30 ng/ml (75 nmol/L)
Based on current research, it seems that consuming 1,000–4,000 IU (25–100 mcg) of vitamin D daily should be ideal for most people to reach healthy vitamin D blood levels.
Instead, a European research team suggests boosting the recommended daily amount to 2,000 IU to combat the risk of certain musculoskeletal diseases, such as rickets or osteomalacia (softening of the bones), or extraskeletal issues such as cancer.
The new recommended daily dose of vitamin D seeks to get a person to a base serum concentration level between at least 50 nanomoles per liter (nmol/L) and 75 nmol/L. The study reports that up to 18 percent of people globally fall below 25 nmol/L, and up to nearly half the world’s population falls below 50 nmol/L. According to the Cleveland Clinic, about 1 billion people worldwide have vitamin D deficiency; in the United States, about 35 percent of the population is deficient.
Vitamin D Needs Are Underestimated by a Factor of 10
This is why it's so important to get your vitamin D level tested at regular intervals. You simply cannot go by dosage. In reality, you should take whatever dosage required to get the vitamin D level in your blood into a healthy range.
According to a study in Anticancer Research (R), it would require 9,600 IUs of vitamin D per day to get a majority (97.5%) of the population to reach 40 ng/mL (100 nmol/L), which research suggests is the very low end of sufficiency (R). That's a far cry from the 600 IUs recommended by the Institute of Medicine (IOM).
One reason why the public has been misled on the issue of dosage stems from a simple mathematical error that has never been corrected. As pointed out in a 2014 paper, the IOM actually underestimates the need by a factor of 10 due to a simple mathematical error. If this error in calculation were to be corrected, the official IOM recommendation would actually be 6,000 IUs a day, not 600 IUs.
You can use a simple tool from GrassrootsHealth to calculate the estimated additional vitamin D intake needed to reach your targeted vitamin D serum level.
According to data published in the Archives of Internal Medicine, 75% of American adults and teens are deficient in vitamin D, based on a sufficiency level of 30 ng/mL. If the sufficiency cutoff were to be moved to 40 or 60 ng/mL, deficiency rates in the U.S. would likely be in the high 90% bracket.
Even with a sufficiency level of 30 ng/mL, 97% of African-Americans and 90% of Mexican-Americans are deficient in this crucial nutrient, which places them at increased risk of chronic disease.
Vitamin D, Calcium, Magnesium and Vitamin K2
When supplementing, also remember to take synergistic effects with other nutrients into account. If you take high-dose vitamin D, you may also need to increase your intake of:- Magnesium
- Vitamin K2
- Calcium
- Excessive vitamin D in combination with lack of vitamin K2 may cause over-absorption of calcium, which in turn may result in calcium deposits in your heart and kidneys. Part of the explanation for these adverse side effects is that vitamin K2 keeps calcium in its appropriate place — in your teeth and bones and out of soft tissues and arteries.
- How much K2 MK7 should i take with vitamin D3? While the optimal ratios between vitamin D and vitamin K2 have yet to be established, taking somewhere between 100 to 200 micrograms (mcg) of K2 is beneficial. Telltale signs of vitamin K2 insufficiency include osteoporosis, heart disease and diabetes. You’re also more likely to be deficient if you rarely eat vitamin K2-rich foods.
- Vascular calcification is also a side effect of low magnesium, so when taking vitamin D3, you need both vitamin K2 and magnesium to make sure everything is working properly.
- Maintaining an appropriate calcium-to-magnesium ratio is also important, as magnesium helps keep calcium in your cells so they can function better. Based on your personal health needs an ideal ratio of calcium-to-magnesium may vary from 1-to-1 to an optimal 1-to-2. (R)
- Magnesium and vitamin K2 also complement each other, as magnesium helps lower blood pressure, which is an important component of heart disease.
Effect of Vitamin D3 Supplements on Development of Advanced Cancer: A Secondary Analysis of the VITAL Randomized Clinical Trial
And those who were of a healthy weight were even more likely to benefit, with a risk reduction of 38 percent.
Vitamin D is primarily known for helping to regulate calcium and phosphate, minerals that are key to developing and maintaining healthy bones, teeth and muscles.
But in recent years, there's been mounting evidence the vitamin D - which we primarily absorb from sunlight - is also involved in the life cycle and growth of many types of cells, including those that make up the immune system.
The Harvard research, published in the JAMA Network Open medical journal (2020), overturns the initial findings of a study of 25,000 people published in 2018.
Initially researchers believed there was no benefit from taking vitamin D, as they detected no reduced incidence of cancer diagnoses overall.
But they were puzzled because cancer deaths went down among those taking the supplements. Meaning, there was no benefit in terms of prevention of cancer but a reduction in cancer deaths was observed.
A secondary analysis, found this anomaly can be explained by the fact that vitamin D seems to stop metastatic cancers - those aggressive types which spread to other parts of the body.Researcher Dr Paulette Chandler, a primary care physician and epidemiologist at Harvard's Brigham And Women's Hospital in Boston, said: 'Vitamin D is a supplement that's readily available, cheap and has been used and studied for decades.
'Our findings, especially the strong risk reduction seen in individuals with normal weight, provide new information about the relationship between vitamin D and advanced cancer.'
More than 25,000 people took part in the study, which spanned more than five years.
The participants included men aged 50 or above and women 55 or older who did not have cancer when the trial began.
The test subjects were divided into four groups - the first group took a daily dose of vitamin D along with omega-3s; the second group took vitamin D plus a dummy placebo, the third consumed omega-3s plus placebo, while the fourth group only had placebos.
The initial results showed no statistical difference in overall cancer rates but a reduction in cancer-related deaths was observed.
In their secondary analysis, Dr Chandler and colleagues evaluated the risk of developing advanced cancer - late-stage and metastatic forms of the disease- among participants who did or did not take vitamin D supplements during the trial.
They also examined whether an individual's body mass index played a role.
Among the participants, 1,617 were diagnosed with an invasive form of cancer - such as breast, prostate, colorectal, lung - over the next five years.
Among those who received vitamin D, 226 were diagnosed with advanced cancer, compared to 274 who received the placebo.
Of those of a healthy weight who took vitamin D, 58 people were diagnosed with advanced cancer compared with 96 taking the placebo.
The team said they found no association between omega-3 fatty acid supplementation and advanced cancer.
The researchers believe obesity and associated inflammation may decrease the effectiveness of vitamin D.
Dr Chandler said: 'Our findings, along with results from previous studies, support the ongoing evaluation of vitamin D supplementation for preventing metastatic cancer - a connection that is biologically plausible.
'Additional studies focusing on cancer patients and investigating the role of BMI are warranted.'
Like Harvard's, most research on vitamin D and cancer shows a link between people who get enough of the vitamin and lower rates of the disease, less aggressive cancers and lower risks of dying from the disease.
But what exactly is going on between vitamin D and cancer - or, for that matter, coronavirus - remains unclear.
In lab studies, pitting vitamin D against cancer cells showed that it can reduce their growth and keep them from multiplying and spreading.This may have to do with the role vitamin D plays in the life cycle of cells, and killing off unhealthy ones - but scientists are still studying whether what they've seen in the confines of a petri dish is true in the human body as well.
Most Vitamin D-Deficient People Are at Increased Risk of Cancer
Generally speaking, research has shown that once you reach a serum vitamin D level of 40 ng/mL, your risk for cancer diminishes by 67%, compared to having a level of 20 ng/ml or less.13,14,15,16,17,18,19 Research shows most cancers occur in people with a vitamin D blood level between 10 and 40 ng/mL, and the optimal level for cancer protection has been identified as being between 40 and 60 ng/mL.20
Vitamin D also increases your chances of surviving cancer if you do get it,21,22 and this includes melanoma, the most dangerous form of skin cancer.23 There's also evidence it can improve treatment outcomes. For example, adding vitamin D to the conventional treatment for pancreatic cancer was found to boost the effectiveness of the treatment.24 It also plays a significant part in protecting you from COVID-1925 and protects you from autoimmune diseases.26,27
Vitamin D Deficiency Linked to Colorectal Cancer
In a 2018 study, researchers found an inverse relationship between vitamin D and colorectal cancer,28 which in 2022 is the third leading cancer killer29 in the U.S. The vitamin D levels of 5,700 colorectal cancer patients in the U.S., Europe and Asia were compared to 7,100 cancer-free controls.
Here, a vitamin D level of 12 ng/mL (30 nmol/L) or less was considered a deficiency state; 20 to 25 ng/mL (50 to 62.5 nmol/L) was considered sufficient for bone health. Far higher levels were associated with cancer protection:
- People with a vitamin D level of 12 ng/mL or below had a 31% higher risk for colorectal cancer compared to those with levels between 20 and 25 ng/mL
- Those with levels between 30 and 35 ng/mL had a 19% reduced risk for colorectal cancer
- Those with levels between 35 and 40 ng/mL had a 27% reduced risk
- For each 10 ng/mL increase in circulating vitamin D, the risk for colorectal cancer was reduced by 19% in women and 7% in men
Coauthor Marji L. McCullough commented on the results, saying,30 "This study adds new information that agencies can use when reviewing evidence for vitamin D guidance and suggests that the concentrations recommended for bone health may be lower than would be optimal for colorectal cancer prevention."
Another study31 published in 2015 found women with vitamin D concentrations of at least 30 ng/mL had a 55% lower risk of colorectal cancer than those who had a blood level below 18 ng/mL. And, a 2019 study showed that high-dose vitamin D benefits patients with advanced metastatic colorectal cancer.32
Vitamin D Protects Against Breast Cancer
Several studies also show that higher vitamin D levels are protective against breast cancer specifically, which is a serious concern for most women. For example, in a 2005 study,33 women with vitamin D levels above 60 ng/mL had an 83% lower risk of breast cancer than those below 20 ng/mL.
More recently, a pooled analysis of two randomized trials and a prospective cohort study again confirmed the link between vitamin D and breast cancer risk.34
The objective was to assess whether there are any benefits to having a vitamin D level above 40 ng/mL, as most studies do not venture into these higher levels. Indeed, mirroring the 2005 findings, women with vitamin D levels at or above 60 ng/mL had an 82% lower incidence rate of breast cancer than those with levels of 20 ng/mL or less.
Pooled data was analyzed in three different ways. First, incidence rates were compared based on vitamin D levels ranging from 20 to 60 ng/mL. Next, statistical analysis using Kaplan-Meier plots were done. Third, multivariate Cox regression was used to examine the association between various vitamin D levels and breast cancer risk. According to the authors:
"Results were similar for the three analyses. First, comparing incidence rates, there was an 82% lower incidence rate of breast cancer for women with 25(OH)D concentrations ≥60 vs <20 ng/mL.Second, Kaplan-Meier curves for concentrations of <20, 20–39, 40–59 and ≥60 ng/mL were significantly different, with the highest proportion breast cancer-free in the ≥60 ng/ml group (99.3%) and the lowest proportion breast cancer-free in the <20 ng/ml group (96.8%). The proportion with breast cancer was 78% lower for ≥60 vs <20 ng/mL.
Third, multivariate Cox regression revealed that women with 25(OH)D concentrations ≥60 ng/ml had an 80% lower risk of breast cancer than women with concentrations <20 ng/mL, adjusting for age, BMI, smoking status, calcium supplement intake, and study of origin … Higher 25(OH)D concentrations were associated with a dose-response decrease in breast cancer risk with concentrations ≥60 ng/mL being most protective."
DO-HEALTH Trial (Cancer Prevention)
Vitamin D Reduces Lung Cancer Death
Vitamin D and Chemotherapy
Vitamin D Deficiency Linked to Lung Disease
We might now consider adding vitamin D deficiency to the list of factors involved in disease processes, along with the known ILD risk factors such as environmental toxins and smoking."
Vitamin D Deficiency Linked to Pregnancy Loss
Vitamin D is perhaps particularly crucial for pregnant women, to protect both their health and the health of their babies. Interestingly, recent research (37,38) suggests vitamin D plays an important role in preventing an adverse immune response against the fetus that might cause her body to reject it as foreign tissue.As noted by the authors, "It stands to reason that an immunocompetent mother would muster an immune response against the fetus. Nevertheless, in reality this does not occur due to various fetomaternal interactions which induce tolerance … Recently, it has come to light that vitamin D may play an integral part in the induction and regulation of this critical immune tolerance process."
What they discovered is that recurrent pregnancy loss, which affects about 1% of couples trying to conceive, is linked to low vitamin D. In short, vitamin D promotes a favorable environment for pregnancy, in part by regulating immune cell differentiation and the excretion of inflammatory cytokines.
According to the authors, "It seems that vitamin D deficiency sways the balance toward a worse outcome and may play a part in recurrent pregnancy loss." Vitamin D also performs many other important functions during pregnancy, and has been shown to dramatically lower a woman's risk for complications and premature birth.
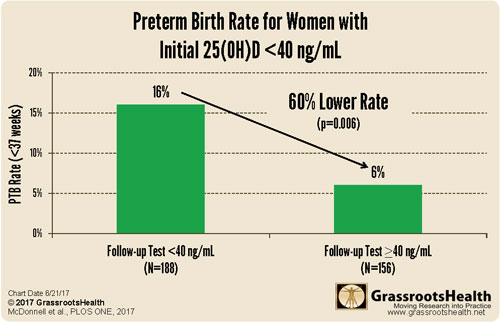
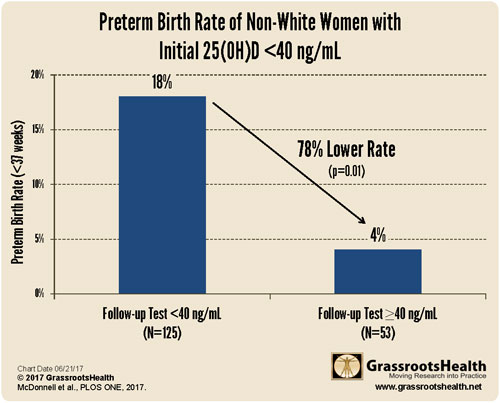
Vitamin D Significantly Lowers Risk of Preterm Birth
Overall, evidence shows pregnant women with a vitamin D level between 40 and 60 ng/mL have 46% lower preterm birth rate than the general population, while those with a vitamin D level at or above 40 ng/mL by their third trimester have a 59% lower risk for premature birth compared to those with levels below 20 ng/mL. (40)
On March 27, 2018, in an effort to break the silence, the Organic & Natural Health Association submitted a health claim petition for vitamin D and preterm birth to the U.S. Food and Drug Administration,(44) the key message being that vitamin D supplementation "directly impacts health outcomes and is changing the standards of care, in this case, for pregnant women and a generation of children."
Vitamin D for Skin Health
Apart from its role in maintaining bone health, vitamin D also has a role in maintaining skin health.
Vitamin D for Dry or Itchy SkinSevere dryness of the skin or Itchy skin can be an indicator of Vitamin D deficiency. Getting enough Vitamin D can improve symptoms of skin disorders that cause dry, itchy skin.
Vitamin D and Psoriasis
Nutritionists are particularly interested in vitamin D supplementation for these two reasons. First, oral vitamin D supplementation is an important supplementary therapeutic choice for psoriatic patients. Second, vitamin D supplementation may be crucial in preventing psoriasis-related comorbidity, hypertension, and metabolic syndrome.
Vitamin D and Vitiligo
According to one study, high-dose vitamin D therapy may be both safe and beneficial in the treatment of vitiligo. Sixteen vitiligo patients with low vitamin D status were given 35,000 IU per day for six months, along with a dairy and calcium-rich food limitation and minimum hydration of 2.5 L per day. And the outcome, fourteen of them had re-pigmentation ranging from 25 to 75%. It’s still uncertain if high-dose supplementation provides any benefits for long-term patients with vitiligo.
Vitamin D and Atopic Dermatitis
Vitamin D may play a role in improving the symptoms of Atopic Dermatitis. The findings of this study imply that vitamin D supplementation may help reduce the severity of atopic dermatitis and can be considered as safe and manageable treatment option. However, this conclusion still needs larger-scale studies over a longer duration of treatment.
Sources and References
- 1 Nutrients 2014; 6(10): 4472-4475
- 2 GrassrootsHealth, 71 % Reduction in All Cancer Risk
- 3 Int J Epidemiol1990;19 (3) 559- 563
- 4 Diabetes Care 2004;27 (12) 2813- 2818
- 5 Chest 2005;128 (6) 3792- 3798
- 6 Am J Clin Nutr 2006;84 (1) 18- 28
- 7 Am J Prev Med 2007;32 (3) 210- 216
- 8 J Steroid Biochem Mol Biol 2007;103 (3-5) 708- 711
- 9, 34 PLOS ONE June 15, 2018
- 10 Anticancer Research 2011 Feb;31(2):607-11
- 11 GrassrootsHealth, Vitamin D Response Curve
- 12 Archives of Internal Medicine 2009;169(6):626-632
- 13 PLOS ONE 2016; 11 (4): e0152441
- 14 PR Web April 6, 2016
- 15 UC San Diego Health April 6, 2016
- 16 Science World Report April 13, 2016
- 17 Oncology Nurse Advisor April 22, 2016
- 18 Tech Times April 11, 2016
- 19 Chrisbeatcancer.com, Vitamin D
- 20 GrassrootsHealth March 24, 2021
- 21 Anticancer Research February 2011: 31(2); 607-611
- 22 UC San Diego Health System Press Release March 6, 2014
- 23 Cancer Network March 21, 2016
- 24 Salk 2022 FAQ on Pancreatic Cancer and Vitamin D
- 25 Chiropractic Economics January 27, 2022
- 26 GrassrootsHealth February 17, 2022
- 27 Frontiers in Endocrinology March 31, 2021
- 28 Journal of the National Cancer Institute June 14, 2018
- 29 National Cancer Institute April 22, 2021
- 30 Eurekalert June 14, 2018
- 31 Cancer Prev Res (Phila). 2015 Aug;8(8):675-82
- 32 Dana-Farber Cancer Institute April 9, 2019
- 33 European Journal of Cancer 2005 May;41(8):1164-9
- 35 The Journal of Nutrition June 19, 2018; nxy066
- 36 Medical News Today June 20, 2018
- 37 Journal of the American Society for Reproductive Immunology June 19, 2018
- 38 Eurekalert June 20, 2018
- 39 Grassrootshealth.org Graphic (PDF)
- 40 Journal of Steroid Biochemistry and Molecular Biology November 10, 2015 [Epub ahead of print]
- 41 PR Web November 20, 2015
- 42, 43 GrassrootsHealth, Research to Support FDA Petition
- 44 Organic & Natural Health Association, Petition for Vitamin D, Preterm Birth Health Claim, March 28, 2018

.png)
.png)






Comments
Post a Comment