In these past few years, stem cells and PRP (platelet-rich plasma) have been hot topics among researchers and doctors. However, these forms of treatments are often mixed up and are confusing for most average consumers.
As of January 2024, there are more than 300,000 studies related to "stem cell" and more than 14,000 studies related to PRP on PubMed (US NIH Library of Medicine Database).
Nevertheless, stem cell and PRP-related therapies are not yet established as standard treatments, given their relatively recent emergence.
Regenerative medicine is also becoming a buzzword in the medical community. Why? Because the human body is specially equipped to heal itself, and regenerative therapies tap into this powerful ability.
Regenerative medicine includes treatments like stem cell therapy and platelet-rich plasma (PRP) therapy. Research around these therapies is expanding every day and it's not easy to keep updated.
We will cover the essentials, differences and explain about each of these biologics below.
PRP is an abbreviation for Platelet Rich Plasma. It is a substance that’s thought to promote healing when injected. Plasma is a component of your blood that contains special “factors,” or proteins, that help your blood to clot. It also contains proteins that support cell growth. Researchers have produced PRP by isolating plasma from blood and concentrating it.
The idea is that injecting PRP into damaged tissues will stimulate your body to grow new, healthy cells and promote healing. Because the tissue growth factors are more concentrated in the prepared growth injections, researchers think the body’s tissues may heal faster. Famous athletes like Tiger Woods and tennis star Rafael Nadal have been known to use these injections to help heal injuries.
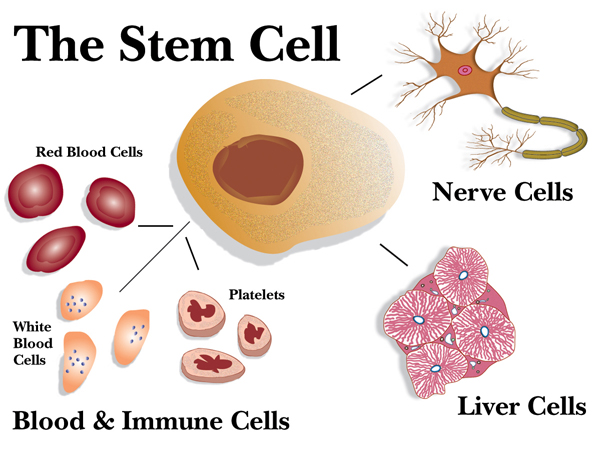
What are Stem Cells?
The primary purpose of stem cells is to maintain, heal and regenerate tissues wherever they reside in your body. This is a continuous process that occurs inside your body throughout your life. If you didn’t have stem cells, your lifespan would be about an hour, because there would be nothing to replace exhausted cells or damaged tissue. In addition, any time your body is exposed to any sort of toxin, the inflammatory process causes stem cells to swarm the area to repair the damage.
Stem cells differ from other kinds of cells in the body. They are special because of their ability to self-renew, duplicate, regenerate and repair.
If you are new to stem cells, check out stem cell basics.
Stem cell treatment, also known as regenerative medicine, uses stem cells or their derivatives to promote the repair response of damaged, dysfunctional, or wounded tissue. It’s the next step in organ transplantation, and it relies on cells rather than donor organs, which are in short supply.
In a lab, researchers grow stem cells. These stem cells are manipulated to specialize into specific types of cells. And then the specialized cells can be implanted into a person. For instance, if the person has heart disease, these cells could be injected into the heart muscle.
PRP vs Stem Cells
What is the difference between stem cell vs PRP? The major advantage of the use of PRP (Platelet Rich Plasma) for therapeutic applications is the immediate preparation of PRP, which does not require any preservative facilities. PRP is considered safe and natural as the preparation involves using own cells without any further modifications.
Although Stem Cells (SC) have added advantage over PRP-based approach in regenerating the damaged tissue, there are certain concerns in using SC for therapies. SC propensity toward self-renewal and differentiation is highly influenced by their local environment making it difficult to interpret how a population of culture expanded stem cells may behave in the human body. Isolation and characterization of SC are crucial and even the isolated SC may have low survival rates. Culturing of SC without contamination requires highly experienced personnel and sophisticated laboratory settings. The chances of microbial contamination of SC might result in complications, especially in those patients whose immune system is compromised. Careful monitoring and observation of this cell-based therapy are of paramount importance, since evidence has shown that fat-derived MSCs (mesenchymal stem cells) have lost genetic stability over time and were prone to cancer formation (
R). Furthermore, SC-based therapies require regular follow-up to monitor regenerated tissue over a period of complete recovery of a patient.
PRP and Stem Cell (SC) therapy is continuously studied for their regenerative benefit in wound healing, sports medicine and chronic pain treatment. Although their preparation, mechanism and action and efficacy have been shown to be different, studies have shown that both PRP and SC can complement each other and might have an added advantage when used in combination (
R).
For example, PRP offers a suitable microenvironment for Mesenchymal Stem Cells (MSCs) to promote proliferation and differentiation and accelerates wound healing capabilities. Conversely, PRP can be a powerful tool to attract cell populations, such as MSCs, a combination of which provides a promising approach for the treatment. Some of the common injuries that are treated using combinational therapy include – tendonitis, rotator cuff tears, osteoarthritis, spine conditions, arthritic joints, overuse injuries, inflammation from herniated disc and others.
PRP vs Stem cell injections for knee
For peripheral mild to moderate tendon injuries (partial shoulder rotator cuff tears, shoulder labral tears, tennis/golfer’s elbow, carpal tunnel syndrome, mild hip osteoarthritis, hip labral tears, gluteal or hamstring tears, trochanteric bursitis, mild knee osteoarthritis, mild meniscal tears, ankle ligament sprain, plantar fasciitis and others), platelet-rich plasma is usually a good alternative of treatment. The ease of collection and lower cost are advantages. The need for repeated treatments is somewhat of a disadvantage.
If the injuries or osteoarthritis are severe, then stem cells are a better alternative. One advantage of stem cell therapy is the treatments required are less, and potential drawbacks are the cost.
The age of the patient determines whether patient’s own stem cells are used or not. After age 45, the number of stem cells in bone marrow decreases rapidly every year. The general health of the patient also contributes to the number and quality of stem cells in their tissues.
For a patient who is 50 years old or older, while PRP could be useful, a decision on whether internal sources of stem cells or external sources of stem cells (commercially available regenerative cells derived from healthy donors) to be used will need to be considered.
There is a plethora of these commercially available products, ranging from growth factors derived from placental tissues (umbilical cord blood, amniotic fluid, Wharton’s jelly, etc) to stem cells derived from donors.
Exosomes are the result of a purification process of stem cells. The result is a concentration of proteins, messenger RNA (mRNA) and growth factors, without any of the original cell’s DNA. The lack of DNA makes rejection of these cells impossible so it lowers the risk of their use.
Can the exosomes found in PRP repair cartilage by themselves? Researchers in Asia (
R) made PRP and then also isolated the exosomes from PRP. They exposed both mixes to cartilage cells and looked at things like cell growth, the ability to close a tear or gap, helping cartilage cells deal with bad inflammation, and resisting apoptosis (cell death). The PRP and the PRP-derived exosomes without platelets performed similarly. Interestingly, the exosomes did better in some tasks, but that result should be taken with a grain of salt as the exosomes were more concentrated than those found in the PRP sample.
Therefore, for an older patient with moderate osteoarthritis, a combination of patient’s own PRP and commercially available exosomes might be a viable and balanced option.
Take Home Messages
It is beyond the scope of this article to describe exactly which treatment is better for which condition. Each patient should be treated like an individual and each treatment should be personalized. The choice of regenerative cells is highly individualized based on age and health of the patient and the extent of injury or degeneration.
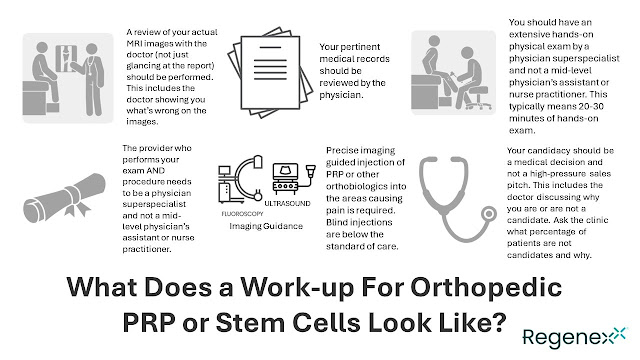
Ultimately, nothing can substitute a thorough evaluation, history, physical examination and a diagnostic work-up. We hope that you keep these things in mind when you seek regenerative treatments anywhere.
Related:
BEST STEM CELL THERAPY CLINICS IN US AND THE WORLD
.png)

.png)



.png)


Comments
Post a Comment