10 Best Natural Anti Inflammatory Supplements of 2023
What is Inflammation?
Your immune system is triggered when your body is exposed to a pathogen (such as viruses, bacteria, or toxic substances) or sustains damage. Inflammatory cells and cytokines are the first responders that your immune system sends out.
In order to trap bacteria and other harmful substances or to begin healing damaged tissue, these cells produce an inflammatory response. As a result, you may experience pain, bruising, swelling, or redness. Inflammation, however, also affects body systems.
Acute Inflammation vs Chronic Inflammation
Acute inflammation is an immediate, adaptive response that can be brought on by a number of unpleasant stimuli including infection and tissue injury.
But if your body releases inflammatory cells even when you are healthy or uninjured, you may have chronic inflammation. For instance, in rheumatoid arthritis, inflammatory cells and substances attack the joint tissues, causing an irregular inflammation that can seriously harm joints and result in pain and deformity.
When Should I Consult the Doctor About Inflammation?
If inflammatory cells stay too long, it may result in chronic inflammation. Chronic inflammation is a symptom of other medical conditions, for instance, rheumatoid arthritis.
Therefore, it is advised that you consult your healthcare practitioner if you have a concerning injury. If you experience persistent pain, bruising, stiffness, or other symptoms, speak with your healthcare professional as well. A healthcare professional can identify the root problem and identify treatments that will make you feel better.
How Can I Get Rid of Inflammation?
– Anti-Inflammatory Diet
Researchers have identified certain foods that can help control inflammation. Many of them are found in the so-called Mediterranean diet, which emphasizes fish, vegetables and olive oil, among other staples.There’s a standardized research tool that’s updated regularly that allows anybody to see if they’re eating foods we know cause chronic inflammation. This is called the The Dietary Inflammatory Index or DII. The choices of pro-inflammatory foods were initially based on studies showing that certain foods like trans-fatty acids (unsaturated fats) caused a spike in serum inflammatory markers in people.
– Autoimmune Protocol Diet
The Autoimmune Protocol (AIP) is a diet that aims to reduce inflammation, pain, and other symptoms caused by autoimmune diseases, such as lupus, inflammatory bowel disease (IBD), celiac disease, and rheumatoid arthritis (Pubmed).Many people who have followed the AIP diet report improvements in the way they feel, as well as reductions in common symptoms of autoimmune disorders, such as fatigue and gut or joint pain. Yet, while research on this diet is promising, it’s also limited.
The AIP diet is an elimination diet designed to help reduce inflammation or other symptoms caused by autoimmune disorders.
It’s comprised of two phases designed to help you identify and ultimately avoid the foods that may trigger inflammation and disease-specific symptoms. Research on its efficacy is limited but appears promising.
Due to its limited downsides, people with autoimmune disorders generally have little to lose by giving it a try. However, it’s likely best to seek guidance from a qualified health professional to ensure you continue to meet your nutrient needs throughout all phases of this diet.
- Control Blood Sugar
It has been hypothesized that consuming a lot of added sugars and sugar-sweetened beverages (SSBs) can promote chronic inflammation. It is best to restrict or stay away from simple carbs like white rice, white flour, refined sugar, and anything that contains high fructose corn syrup.
- Exercise/Physical Activity
Consistent data from observational studies showing a link between self-reported levels of physical activity and inflammatory biomarkers, as well as some promising positive data from randomized, controlled trials, indicate that increasing aerobic physical activity could be effective for reducing chronic inflammation, especially in individuals with chronic diseases associated with a state of elevated inflammation. (Source)- Manage Stress
Best Natural Anti-Inflammatory Supplements
1. Omega-3 Fish Oil
Omega-3 fatty acids are essential fats, meaning you must get them from the food you eat, as your body can’t make them.
They’ve been associated with numerous health benefits, such as a reduced risk of heart disease, reduced inflammation, and improved mood (Source, Source, Source).
Fish oil and flaxseed oil each contain an impressive amount of omega-3 fatty acids.
The main types of omega-3s in fish oil are eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) (Source).
On the other hand, flaxseed oil contains the omega-3 fatty acid known as alpha-linoleic acid (ALA) (Trusted Source). Flaxseed oil also contains linoleic acid, an omega-6 fatty acid.
EPA and DHA are predominantly found in animal foods like fatty fish, while ALA is mostly found in plants.
However, ALA isn’t biologically active and needs to be converted to EPA and DHA to be used for something other than just stored energy like other types of fat (Trusted Source).
While ALA is still an essential fatty acid, EPA and DHA are linked to many more health benefits (Trusted Source). Additionally, the conversion process from ALA to EPA and DHA is quite inefficient in humans (Trusted Source). For example, one study found that only 5% of ALA is converted to EPA and less than 0.5% of ALA is converted to DHA in adults (Trusted Source).
EPA and DHA can reduce inflammation, which causes swelling and pain. Research has indicated that both acids might suppress the body’s immune system. However, a 2016 study suggests that DHA might enhance immune function instead. DHA is more effective at reducing inflammation than EPA, but both have a role.
All of these effects makes fish oil potentially beneficial for people with arthritis.
EPA and DHA come with other health benefits: They can help prevent heart attacks by making it harder for blood to clot. They help lower blood triglyceride levels and blood pressure. As well, EPA taken with statin medication is more effective in reducing the inflammation of arteriosclerosis than medication alone.
For the omega-3 fatty acids in fish oil to work against arthritis, it’s necessary to consume a fairly large quantity of it each day. Fish oil — or cod liver oil — enclosed in capsules makes this fairly easy.
On the other hand, because cod liver oil contains very high amounts of vitamin A and vitamin D, taking too much can be toxic. For the purpose of treating arthritis, fish oil is the safer choice.
According to a review (Nutrients, September 2022), data from scientific literature 'overwhelmingly' supports beneficial effects of omega-3 fatty acids on the length of telomeres, reported to be a marker of biological age.
Many governments recommend eating omega-3 containing fatty fish, two times per week. But that is often not enough. Ideally, people would need to eat fatty fish four times per week, while also supplementing with omega-3 fatty acids, at least 1,000 mg of pure omega-3 (DHA and EPA) per day.
Make sure you buy high-quality omega-3 fatty acid supplements, meaning that the omega-3 fatty acids are pure and have not oxidized much (having low “TOTOX” value).
TOTOX value stands for total oxidation value. The omega 3 fatty acids EPA and DHA from fish oil are highly sensitive to oxidation. This means that they are rapidly affected by contact with oxygen. Oxidised fatty acids are not beneficial to our health. For this reason, a good fish oil supplement has a low TOTOX value. The maximum TOTOX value is set at 26 by the Global Organization for EPA and DHA omega-3.
Shop for fish oil supplement.
Omega-3 fatty acids are essential fats, meaning you must get them from the food you eat, as your body can’t make them.
They’ve been associated with numerous health benefits, such as a reduced risk of heart disease, reduced inflammation, and improved mood (Source, Source, Source).
Fish oil and flaxseed oil each contain an impressive amount of omega-3 fatty acids.
The main types of omega-3s in fish oil are eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) (Source).
On the other hand, flaxseed oil contains the omega-3 fatty acid known as alpha-linoleic acid (ALA) (Trusted Source). Flaxseed oil also contains linoleic acid, an omega-6 fatty acid.
They’ve been associated with numerous health benefits, such as a reduced risk of heart disease, reduced inflammation, and improved mood (Source, Source, Source).
Fish oil and flaxseed oil each contain an impressive amount of omega-3 fatty acids.
The main types of omega-3s in fish oil are eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) (Source).
On the other hand, flaxseed oil contains the omega-3 fatty acid known as alpha-linoleic acid (ALA) (Trusted Source). Flaxseed oil also contains linoleic acid, an omega-6 fatty acid.
EPA and DHA are predominantly found in animal foods like fatty fish, while ALA is mostly found in plants.
However, ALA isn’t biologically active and needs to be converted to EPA and DHA to be used for something other than just stored energy like other types of fat (Trusted Source).
While ALA is still an essential fatty acid, EPA and DHA are linked to many more health benefits (Trusted Source). Additionally, the conversion process from ALA to EPA and DHA is quite inefficient in humans (Trusted Source). For example, one study found that only 5% of ALA is converted to EPA and less than 0.5% of ALA is converted to DHA in adults (Trusted Source).
EPA and DHA can reduce inflammation, which causes swelling and pain. Research has indicated that both acids might suppress the body’s immune system. However, a 2016 study suggests that DHA might enhance immune function instead. DHA is more effective at reducing inflammation than EPA, but both have a role.
All of these effects makes fish oil potentially beneficial for people with arthritis.
EPA and DHA come with other health benefits: They can help prevent heart attacks by making it harder for blood to clot. They help lower blood triglyceride levels and blood pressure. As well, EPA taken with statin medication is more effective in reducing the inflammation of arteriosclerosis than medication alone.
For the omega-3 fatty acids in fish oil to work against arthritis, it’s necessary to consume a fairly large quantity of it each day. Fish oil — or cod liver oil — enclosed in capsules makes this fairly easy.
On the other hand, because cod liver oil contains very high amounts of vitamin A and vitamin D, taking too much can be toxic. For the purpose of treating arthritis, fish oil is the safer choice.
According to a review (Nutrients, September 2022), data from scientific literature 'overwhelmingly' supports beneficial effects of omega-3 fatty acids on the length of telomeres, reported to be a marker of biological age.
Many governments recommend eating omega-3 containing fatty fish, two times per week. But that is often not enough. Ideally, people would need to eat fatty fish four times per week, while also supplementing with omega-3 fatty acids, at least 1,000 mg of pure omega-3 (DHA and EPA) per day.
Make sure you buy high-quality omega-3 fatty acid supplements, meaning that the omega-3 fatty acids are pure and have not oxidized much (having low “TOTOX” value).
Many governments recommend eating omega-3 containing fatty fish, two times per week. But that is often not enough. Ideally, people would need to eat fatty fish four times per week, while also supplementing with omega-3 fatty acids, at least 1,000 mg of pure omega-3 (DHA and EPA) per day.
Make sure you buy high-quality omega-3 fatty acid supplements, meaning that the omega-3 fatty acids are pure and have not oxidized much (having low “TOTOX” value).
Shop for fish oil supplement.
2. Vitamin D
Perhaps bone health and sunlight is what comes to your mind when you hear “Vitamin D” but very few of us realize vitamin D’s capacity to manage inflammation.
The production of inflammatory proteins (cytokines) and immune cells is better regulated when Vitamin D levels are optimized. This is crucial for preventing the development of many immune-related diseases (R).
In fact, one study showed that individuals with adequate vitamin D levels did not experience the typical inflammatory cascade. Those with subpar vitamin D levels failed to inhibit the inflammatory cascade (R).
Vitamin D3, also known as cholecalciferol, is the best form of vitamin D. D3 is the natural form of vitamin D. It is what our body makes when we are exposed to sunlight.
Eating egg yolks might allow for sufficient vitamin D levels. Be sure to take your D3 with a meal as vitamin D is a fat-soluble vitamin.
The early part of the 21st century brought enormous attention to the importance and value of vitamin D, particularly in the treatment of autoimmune diseases like Rheumatoid Arthritis.
Make sure to take 500 mg to 1000 mg of magnesium and 150 mcg of vitamin K2, (not K1) which are important cofactors for optimizing vitamin D function. And, remember the only way you know what your vitamin D level is, is to test it. Vitamin D level should be in a therapeutic range of 50 to 70 ng/ml for treatment of rheumatoid arthritis. Most people are shocked how low their level is when they finally get around to testing it.
Perhaps bone health and sunlight is what comes to your mind when you hear “Vitamin D” but very few of us realize vitamin D’s capacity to manage inflammation.
The production of inflammatory proteins (cytokines) and immune cells is better regulated when Vitamin D levels are optimized. This is crucial for preventing the development of many immune-related diseases (R).
In fact, one study showed that individuals with adequate vitamin D levels did not experience the typical inflammatory cascade. Those with subpar vitamin D levels failed to inhibit the inflammatory cascade (R).
In fact, one study showed that individuals with adequate vitamin D levels did not experience the typical inflammatory cascade. Those with subpar vitamin D levels failed to inhibit the inflammatory cascade (R).
Vitamin D3, also known as cholecalciferol, is the best form of vitamin D. D3 is the natural form of vitamin D. It is what our body makes when we are exposed to sunlight.
Eating egg yolks might allow for sufficient vitamin D levels. Be sure to take your D3 with a meal as vitamin D is a fat-soluble vitamin.
Eating egg yolks might allow for sufficient vitamin D levels. Be sure to take your D3 with a meal as vitamin D is a fat-soluble vitamin.
Make sure to take 500 mg to 1000 mg of magnesium and 150 mcg of vitamin K2, (not K1) which are important cofactors for optimizing vitamin D function. And, remember the only way you know what your vitamin D level is, is to test it. Vitamin D level should be in a therapeutic range of 50 to 70 ng/ml for treatment of rheumatoid arthritis. Most people are shocked how low their level is when they finally get around to testing it.
3. Turmeric (Curcumin)
Curcumin is an antioxidant that may offer a variety of anti-inflammatory benefits. It’s present in turmeric, a mild spice that can add color and flavor to sweet and savory dishes, as well as teas.
It’s also available as a supplement.
It is somewhat unbelievable how many articles have been published regarding turmeric’s ability to tackle inflammation in the human body. There is data to support just about every condition; Joint paint, digestion, Crohn’s Disease, heart disease, depression, cancer, cognition and eczema to name a few.
Curcumin, present in turmeric, has long played a role in Chinese and Ayurvedic medicine, due to its anti-inflammatory properties.
In 2019, some researchers found that curcumin capsules had a similar effect on the symptoms of knee osteoarthritis as diclofenac, an NSAID.
In the study, 139 people with OsteoArthritis of the knee took either a 50-milligram tablet of diclofenac twice a day for 28 days or a 500-milligram curcumin capsule three times a day.
Both groups said their pain levels improved, but those who took curcumin had fewer negative effects. The research suggested that people who can’t take NSAIDs may be able to use curcumin instead.
You can find curcumin supplements on Amazon.
Curcumin is an antioxidant that may offer a variety of anti-inflammatory benefits. It’s present in turmeric, a mild spice that can add color and flavor to sweet and savory dishes, as well as teas.
It’s also available as a supplement.
It is somewhat unbelievable how many articles have been published regarding turmeric’s ability to tackle inflammation in the human body. There is data to support just about every condition; Joint paint, digestion, Crohn’s Disease, heart disease, depression, cancer, cognition and eczema to name a few.
Curcumin, present in turmeric, has long played a role in Chinese and Ayurvedic medicine, due to its anti-inflammatory properties.
In 2019, some researchers found that curcumin capsules had a similar effect on the symptoms of knee osteoarthritis as diclofenac, an NSAID.
In the study, 139 people with OsteoArthritis of the knee took either a 50-milligram tablet of diclofenac twice a day for 28 days or a 500-milligram curcumin capsule three times a day.
Both groups said their pain levels improved, but those who took curcumin had fewer negative effects. The research suggested that people who can’t take NSAIDs may be able to use curcumin instead.
Curcumin, present in turmeric, has long played a role in Chinese and Ayurvedic medicine, due to its anti-inflammatory properties.
In 2019, some researchers found that curcumin capsules had a similar effect on the symptoms of knee osteoarthritis as diclofenac, an NSAID.
In the study, 139 people with OsteoArthritis of the knee took either a 50-milligram tablet of diclofenac twice a day for 28 days or a 500-milligram curcumin capsule three times a day.
Both groups said their pain levels improved, but those who took curcumin had fewer negative effects. The research suggested that people who can’t take NSAIDs may be able to use curcumin instead.
You can find curcumin supplements on Amazon.
4. Resveratrol, Quercetin and Pterostilbene
Resveratrol is another nutrient that has antioxidant and anti-inflammatory properties.
In a 2018 study, scientists gave 110 people with mild to moderate OA of the knee a 500-milligram dose of resveratrol or a placebo. They took this combination alongside a 15-gram dose of the NSAID meloxicam every day for 90 days.
People who took resveratrol found that their pain levels dropped significantly, compared with those who took the placebo. More research is needed to confirm that resveratrol can benefit people with OA.
However, if you’re already taking another NSAID and it doesn’t reduce your pain as much as you’d like, the research suggests Resveratrol may be a useful add-on.
Quercetin has also been shown to reduce inflammation in multiple studies. In this 8 week study (2017) involving 50 women with rheumatoid arthritis, participants took 500mg of quercetin per day or a placebo. The quercetin group reported less early morning stiffness, morning pain, and after-activity pain.
Early studies on quercetin and inflammation are promising, although more large scale human studies need to be performed to verify these benefits.
Resveratrol is another nutrient that has antioxidant and anti-inflammatory properties.
In a 2018 study, scientists gave 110 people with mild to moderate OA of the knee a 500-milligram dose of resveratrol or a placebo. They took this combination alongside a 15-gram dose of the NSAID meloxicam every day for 90 days.
People who took resveratrol found that their pain levels dropped significantly, compared with those who took the placebo. More research is needed to confirm that resveratrol can benefit people with OA.
However, if you’re already taking another NSAID and it doesn’t reduce your pain as much as you’d like, the research suggests Resveratrol may be a useful add-on.
People who took resveratrol found that their pain levels dropped significantly, compared with those who took the placebo. More research is needed to confirm that resveratrol can benefit people with OA.
However, if you’re already taking another NSAID and it doesn’t reduce your pain as much as you’d like, the research suggests Resveratrol may be a useful add-on.
Quercetin has also been shown to reduce inflammation in multiple studies. In this 8 week study (2017) involving 50 women with rheumatoid arthritis, participants took 500mg of quercetin per day or a placebo. The quercetin group reported less early morning stiffness, morning pain, and after-activity pain.
Early studies on quercetin and inflammation are promising, although more large scale human studies need to be performed to verify these benefits.
Early studies on quercetin and inflammation are promising, although more large scale human studies need to be performed to verify these benefits.
5. Chondroitin and Glucosamine
Many clinical studies have found that chondroitin can reduce joint pain and stiffness in people with osteoarthritis. About 53 percent of people who take chondroitin have a 20 percent or greater improvement in knee pain.
Chondroitin sulfate may also slow down the progression of osteoarthritis when taken long-term. Studies show that it slows down narrowing of the joint space when taken for up to 2 years.
Joint supplements often combine chondroitin with glucosamine. In a 2022 meta-analysis of 8 randomized controlled trials, that included more than 3,700 patients; confirmed that the combination of glucosamine and chondroitin is effective and superior to other treatments in knee osteoarthritis to a certain extent.
Try it: Chondroitin is typically taken in a dose of 400 to 800 mg two or three times per day.
You can find chondroitin supplements on Amazon.
Many clinical studies have found that chondroitin can reduce joint pain and stiffness in people with osteoarthritis. About 53 percent of people who take chondroitin have a 20 percent or greater improvement in knee pain.
Chondroitin sulfate may also slow down the progression of osteoarthritis when taken long-term. Studies show that it slows down narrowing of the joint space when taken for up to 2 years.
Joint supplements often combine chondroitin with glucosamine. In a 2022 meta-analysis of 8 randomized controlled trials, that included more than 3,700 patients; confirmed that the combination of glucosamine and chondroitin is effective and superior to other treatments in knee osteoarthritis to a certain extent.
Try it: Chondroitin is typically taken in a dose of 400 to 800 mg two or three times per day.
Chondroitin sulfate may also slow down the progression of osteoarthritis when taken long-term. Studies show that it slows down narrowing of the joint space when taken for up to 2 years.
Joint supplements often combine chondroitin with glucosamine. In a 2022 meta-analysis of 8 randomized controlled trials, that included more than 3,700 patients; confirmed that the combination of glucosamine and chondroitin is effective and superior to other treatments in knee osteoarthritis to a certain extent.
Try it: Chondroitin is typically taken in a dose of 400 to 800 mg two or three times per day.
You can find chondroitin supplements on Amazon.
6. Glutathione Boosting Agents (NAC)
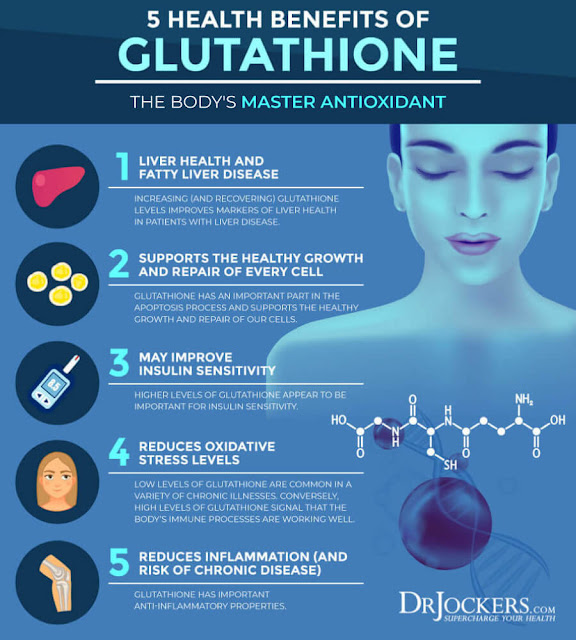
Glutathione is our master antioxidant that regulates all other antioxidants within the body. Having high amounts of glutathione in the body is key for mitigating the inflammatory effects of free radicals.
Free radicals are upregulated during any time of stress whether it is lifestyle or something like a bacterial imbalance in the gut. For clinical applications, we will either use glutathione boosting agents like N-acetyl cysteine (NAC) or acetylated glutathione.
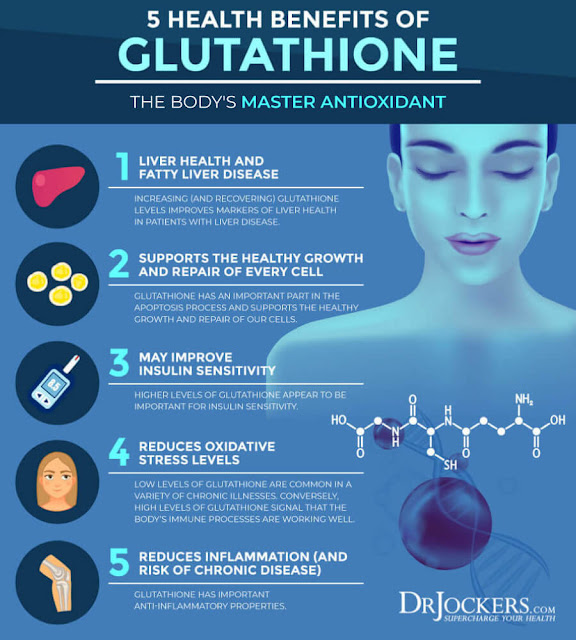
Glutathione is our master antioxidant that regulates all other antioxidants within the body. Having high amounts of glutathione in the body is key for mitigating the inflammatory effects of free radicals.
Free radicals are upregulated during any time of stress whether it is lifestyle or something like a bacterial imbalance in the gut. For clinical applications, we will either use glutathione boosting agents like N-acetyl cysteine (NAC) or acetylated glutathione.
7. Methylsulfonylmethane (MSM)
Methylsulfonylmethane (MSM) is another common ingredient in supplements said to help with joint pain. One of the most popular uses of MSM is to decrease joint or muscle pain. It has been shown to benefit those with joint degeneration, a common cause of pain in the knees, back, hands and hips.
A study in 100 people over the age of 50 found that treatment with a supplement containing 1,200 mg of MSM for 12 weeks decreased pain, stiffness and swelling in the joints, compared to a placebo (Int J Biomed Sci. 2015).
The group receiving the supplement also reported improved overall quality of life and less difficulty walking and getting out of bed (Int J Biomed Sci. 2015).
In one randomised controlled study (2011), MSM improved pain and functioning compared to a placebo in people with osteoarthritis.
Another study in 32 people with lower back pain found that taking a glucosamine supplement containing MSM significantly reduced lumbar stiffness and pain upon movement, plus greatly increased quality of life (Curr Ther Res Clin Exp. 2005).
Try it: Typical MSM doses range from 1,500 to 6,000 grams per day, sometimes divided into two doses.
You can find MSM supplements on Amazon.
Methylsulfonylmethane (MSM) is another common ingredient in supplements said to help with joint pain. One of the most popular uses of MSM is to decrease joint or muscle pain. It has been shown to benefit those with joint degeneration, a common cause of pain in the knees, back, hands and hips.
A study in 100 people over the age of 50 found that treatment with a supplement containing 1,200 mg of MSM for 12 weeks decreased pain, stiffness and swelling in the joints, compared to a placebo (Int J Biomed Sci. 2015).
The group receiving the supplement also reported improved overall quality of life and less difficulty walking and getting out of bed (Int J Biomed Sci. 2015).
A study in 100 people over the age of 50 found that treatment with a supplement containing 1,200 mg of MSM for 12 weeks decreased pain, stiffness and swelling in the joints, compared to a placebo (Int J Biomed Sci. 2015).
The group receiving the supplement also reported improved overall quality of life and less difficulty walking and getting out of bed (Int J Biomed Sci. 2015).
In one randomised controlled study (2011), MSM improved pain and functioning compared to a placebo in people with osteoarthritis.
Another study in 32 people with lower back pain found that taking a glucosamine supplement containing MSM significantly reduced lumbar stiffness and pain upon movement, plus greatly increased quality of life (Curr Ther Res Clin Exp. 2005).
Try it: Typical MSM doses range from 1,500 to 6,000 grams per day, sometimes divided into two doses.
Another study in 32 people with lower back pain found that taking a glucosamine supplement containing MSM significantly reduced lumbar stiffness and pain upon movement, plus greatly increased quality of life (Curr Ther Res Clin Exp. 2005).
Try it: Typical MSM doses range from 1,500 to 6,000 grams per day, sometimes divided into two doses.
You can find MSM supplements on Amazon.
8. Vitamin C
Boosting your vitamin C intake also affects the inflammatory response in the body. Vitamin C is a crucial component of a treatment protocol developed by Dr. Paul Marik, previously a critical care doctor at Sentara Norfolk General Hospital in East Virginia. The treatment protocol was developed for sepsis, which is a life-threatening condition triggered by a systemic infection that causes your body to overreact and launch an excessive and damaging immune response.
According to a 2011 paper, the coagulation system, which is dysfunctional in sepsis, is closely related to the inflammatory response. The communication between the two systems drives the dysregulated response that ultimately results in a very high mortality rate.
Unless sepsis is diagnosed promptly and treated appropriately, it can progress rapidly to multiple organ failure and death. This includes cases of suspected influenza since sepsis can mimic many of the signs and symptoms of flu. Although severe sepsis has traditionally been linked to bacterial infections, doctors are seeing more patients with severe sepsis that are caused directly by influenza viruses.
Marik’s retrospective before-after clinical study showed giving patients 200 mg of thiamine every 12 hours, 1,500 mg of ascorbic acid every six hours, and 50 mg of hydrocortisone every six hours for two days reduced mortality from 40.4% to 8.5%.
As importantly, the treatment has no side effects and is inexpensive, readily available and simple to administer. In other words, there's virtually no risk involved. Research published in 2020 found Marik’s sepsis protocol lowered mortality in pediatric patients as well.
Utilizing vitamin C in the treatment of sepsis may help lower both mortality rate and cost. Each year an estimated 1.7 million Americans get sepsis, and nearly 270,000 of them die.
Conventional treatment focuses on high-dose antibiotics. A U.S. government report published in 2016 noted that sepsis was the most expensive condition treated in the U.S., racking up $23.7 billion in health care costs each year. By 2022, that had skyrocketed to $62 billion just for treatment and care.
Related: How Vitamin C Is Effective in Treating Inflammatory Issues
Boosting your vitamin C intake also affects the inflammatory response in the body. Vitamin C is a crucial component of a treatment protocol developed by Dr. Paul Marik, previously a critical care doctor at Sentara Norfolk General Hospital in East Virginia. The treatment protocol was developed for sepsis, which is a life-threatening condition triggered by a systemic infection that causes your body to overreact and launch an excessive and damaging immune response.
According to a 2011 paper, the coagulation system, which is dysfunctional in sepsis, is closely related to the inflammatory response. The communication between the two systems drives the dysregulated response that ultimately results in a very high mortality rate.
According to a 2011 paper, the coagulation system, which is dysfunctional in sepsis, is closely related to the inflammatory response. The communication between the two systems drives the dysregulated response that ultimately results in a very high mortality rate.
Unless sepsis is diagnosed promptly and treated appropriately, it can progress rapidly to multiple organ failure and death. This includes cases of suspected influenza since sepsis can mimic many of the signs and symptoms of flu. Although severe sepsis has traditionally been linked to bacterial infections, doctors are seeing more patients with severe sepsis that are caused directly by influenza viruses.
Marik’s retrospective before-after clinical study showed giving patients 200 mg of thiamine every 12 hours, 1,500 mg of ascorbic acid every six hours, and 50 mg of hydrocortisone every six hours for two days reduced mortality from 40.4% to 8.5%.
As importantly, the treatment has no side effects and is inexpensive, readily available and simple to administer. In other words, there's virtually no risk involved. Research published in 2020 found Marik’s sepsis protocol lowered mortality in pediatric patients as well.
Utilizing vitamin C in the treatment of sepsis may help lower both mortality rate and cost. Each year an estimated 1.7 million Americans get sepsis, and nearly 270,000 of them die.
Conventional treatment focuses on high-dose antibiotics. A U.S. government report published in 2016 noted that sepsis was the most expensive condition treated in the U.S., racking up $23.7 billion in health care costs each year. By 2022, that had skyrocketed to $62 billion just for treatment and care.
Related: How Vitamin C Is Effective in Treating Inflammatory Issues
Marik’s retrospective before-after clinical study showed giving patients 200 mg of thiamine every 12 hours, 1,500 mg of ascorbic acid every six hours, and 50 mg of hydrocortisone every six hours for two days reduced mortality from 40.4% to 8.5%.
As importantly, the treatment has no side effects and is inexpensive, readily available and simple to administer. In other words, there's virtually no risk involved. Research published in 2020 found Marik’s sepsis protocol lowered mortality in pediatric patients as well.
Utilizing vitamin C in the treatment of sepsis may help lower both mortality rate and cost. Each year an estimated 1.7 million Americans get sepsis, and nearly 270,000 of them die.
Conventional treatment focuses on high-dose antibiotics. A U.S. government report published in 2016 noted that sepsis was the most expensive condition treated in the U.S., racking up $23.7 billion in health care costs each year. By 2022, that had skyrocketed to $62 billion just for treatment and care.
9. Pine Bark Extract (Pycnogenol)
This is a relatively new comer in this anti inflammatory space.
Pine bark acts as a local anti-inflammatory in synovial fluid (R) and three publications have shown it to improve KOA (knee osteoarthritis) pain and stiffness, NSAID (non steroidal anti inflammatory drug) use, physical and emotional well-being (R, R, R). Pine bark preparations have recently been “strongly recommended” to the rheumatology community as early and additive treatment for OA, likely based on the following meta-analysis (R, R).
In a 2020 randomized controlled trial, mineral rich algae with pine bark improved pain, physical function and analgesic use in mild-knee joint osteoarthritis, compared to Glucosamine.
Related: Pycnogenol vs Pine Bark Extract
This is a relatively new comer in this anti inflammatory space.
Pine bark acts as a local anti-inflammatory in synovial fluid (R) and three publications have shown it to improve KOA (knee osteoarthritis) pain and stiffness, NSAID (non steroidal anti inflammatory drug) use, physical and emotional well-being (R, R, R). Pine bark preparations have recently been “strongly recommended” to the rheumatology community as early and additive treatment for OA, likely based on the following meta-analysis (R, R).
10. Zinc
In this review, published in the Journal of Trace Elements in Medicine and Biology (2014), zinc is also an antioxidant and anti-inflammatory agent. Zinc supplementation studies in the elderly have shown decreased incidence of infections, decreased oxidative stress, and decreased generation of inflammatory cytokines. Decreased incidences of blindness in patients with AMD and increased atheroprotective effect have been observed in the zinc supplemented elderly.
Note: Atheroprotective effect means to prevent plaque within the blood vessels.
In this review, published in the Journal of Trace Elements in Medicine and Biology (2014), zinc is also an antioxidant and anti-inflammatory agent. Zinc supplementation studies in the elderly have shown decreased incidence of infections, decreased oxidative stress, and decreased generation of inflammatory cytokines. Decreased incidences of blindness in patients with AMD and increased atheroprotective effect have been observed in the zinc supplemented elderly.
Note: Atheroprotective effect means to prevent plaque within the blood vessels.
.png)

.png)




.png)

Comments
Post a Comment