Can Things Like Lyme, Mold, COVID, or Your Diet Destroy Your Ligaments?
Functional Medicine Diagnoses
The purpose of this blog isn’t to get into the extensive controversy over whether chronic Lyme or mold-caused illnesses (CIRS) or any of these other diagnoses are valid. The traditional medical community doesn’t like many of these diagnoses which are staples of the functional medicine community. For my entire career, I have worked with patients who are comfortable being treated in both worlds. My goal with today’s blog is to explore the science behind whether we can draw a connection between these diagnoses and ligament damage. Hence, I will be looking for basic science studies done in the lab or in animal models that tie these two things together, knowing that the clinical research on these topics and ligaments is nonexistent.Traditional Medicine?
If you read these blogs on a regular basis, you know that I am not a fanboy of traditional medicine. In fact, I’m often openly critical of the way most traditional MDs approach things like arthritis, ligament laxity, spinal pain, etc… Having said that, I am a fan of trying to use the science we have to support how you diagnose and treat a patient. That doesn’t mean that we need Randomized Controlled Trials (RCTs) to support every clinical decision. Anybody who does that, in my opinion, is an awful clinician. That’s because these RCTs don’t exist for most of the decisions physicians make every day and using that rule just creates a physician locked into “Analysis Paralysis” mode.
Today we’ll be diving into what’s published in the US National Library of Medicine. This is NOT a tool for traditional medicine, certainly not at the level of basic science and animal studies. In fact, many in the functional medicine world use these same studies found in this library to support their theories on diagnosis and treatment.
Who are These Patients?
The patients I speak to most these days who are concerned about ligament damage and infections/exposures are trying to determine if they have CCI (Craniocervical Instability). This means that there has been damage to the ligaments that hold their head on causing lots of different symptoms including headache, dizziness, neck pain, and autonomic dysfunction. While this patient type has usually had some sort of head/neck trauma or has hEDS (born with overly stretchy ligaments), these infection/exposure patients don’t have this history and have usually been told by a functional medicine doctor or have read on social media sites that their ligaments are degenerating because of these factors.
Today we’ll cover some of the causes I have been given in these Telemedicine visits for why these patients have CCI:
- Chronic Lyme Disease
- Mold Exposure (CIRS)
- COVID-19
- MCAS
- Diet
- Chronic Inflammation
The Basic Concepts
The two ideas we’ll be dealing with today are ligament damage due to a pathogen eating away at connective tissue and damaging inflammation.
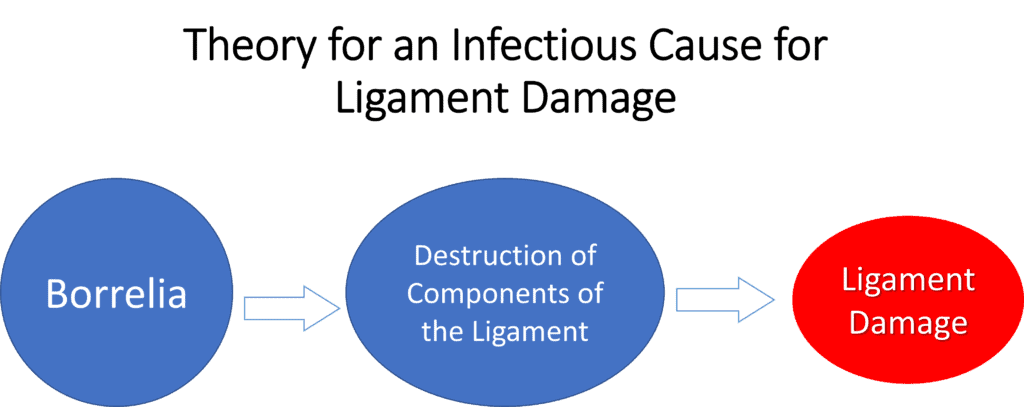
This is what the first theory looks like:
Here an infectious pathogen like Borrelia destroys ligaments by eating away at components of that structure.
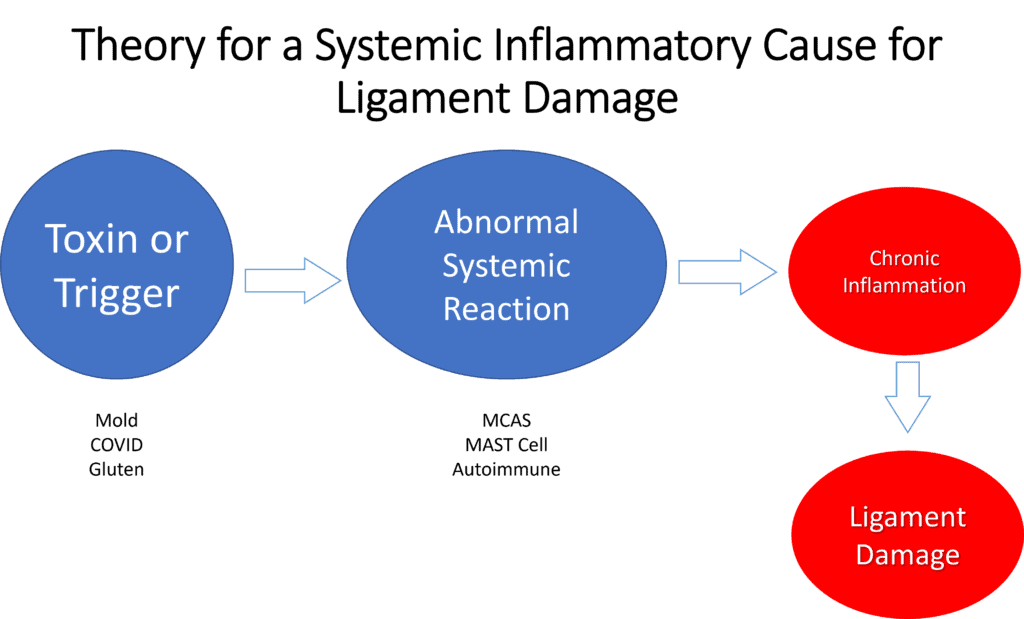
The second theory we’ll be covering today looks like this:
Here, some environmental or dietary trigger causes an abnormal immune system to respond with excessive inflammation which leads to ligament damage.
Remember, both of these are THEORIES without definitive scientific proof at this time.
Chronic Lyme Disease and Ligaments
The idea behind chronic Lyme disease is that a tick bite infects the patient with one of four species of the Borrelia spirochete. Acute and sub-acute Lyme infection can cause all sorts of issues from rashes to joint pain to neurologic symptoms. The more controversial issue is whether a long-term or chronic Lyme infection exists and whether that can cause widespread lifetime damage throughout the body. However, the task at hand here this morning is to determine if we have research connecting these Borrelia infections to ligament damage.
I searched the US National Library of Medicine for basic science studies for “Borrelia Ligament”. In published opinion/review pieces, I dove into the references in those publications and included any that seemed to show a credible link. This is what I found:
- A European dog study looked at Cranial Cruciate Ligament rupture (CCL) and Borrelia (and other vector-borne pathogens). No relationship was found between these pathogens and ligament rupture. (1) A lower-level canine case series did find a relationship between Borrelia and CCL rupture (4).
- A single case study of a patient who had Lyme spirochetes cultured from her ligament samples taken during a trigger finger surgery. (2)
- A case series report in German that connected C1-C2 instability (unknown if this was CCI or how that diagnosis was rendered) in some percentage of the cases examined who had chronic IgG antibodies to Borrelia and evidence of white blood cell sensitization to the same (LTT). (3) Functional MRIs were performed, but the exact data from those images was not really reported.
BOTTOM LINE: As far as convincing human research, there is one case series (lower level evidence) of patients who had been diagnosed with CCI, and various tests for the body’s response to Borrelia were positive, but this did not include a control group so we don’t know how positive these tests would have been in random people from the local population. In addition, how CCI was diagnosed in this study is unknown. So is there a clear connection between chronic Lyme and ligament damage? There’s one study that looks interesting, but this is not in any way definitive.
Mold Exposure (CIRS)
The general concept behind mold exposure is that the patient lives in a home where water damage which leads to mold growth and that patient has the right genetic and environmental makeup to react to this exposure by producing a chronic inflammatory state. This syndrome goes by the name Chronic Inflammatory Response Syndrome (CIRS).
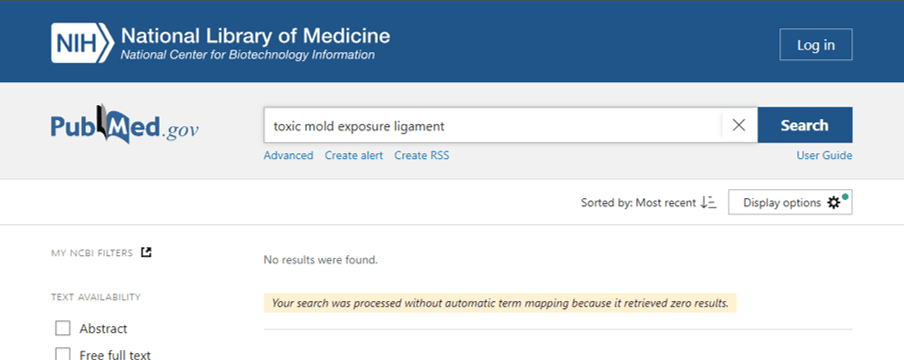
I again did a search through the US National library of medicine, but regrettably found nothing linking mold to ligament damage:
BOTTOM LINE: We have no scientific research linking mold exposure to ligament damage.
COVID-19
Some patients of late have focused on COVID-19 as a cause for their ligament problems. However, what we know for sure in this area is still evolving. Here’s what I found:
- It’s currently believed that pre-existing musculoskeletal problems are made worse during the hyper-inflammatory response that happens in a small subset of COVID-19-infected patients. (5)
- Musculoskeletal complaints are common with long-COVID, but nobody knows if this is due to inactivity or some aspect of the syndrome since long COVID is currently poorly defined as a diagnosis. (6)
- Our understanding of this phenomenon is rudimentary at best-meaning no cases of ligament damage caused by COVID have been described in the scientific literature.
BOTTOM LINE: We have no scientific research linking COVID-19 to ligament damage.
MCAS
Mast Cell Activation Syndrome (MCAS) is a condition where people experience repeated episodes of allergic reactions due to excessive mast cell activity (7). These sensitized cells dump abnormally high levels of cytokines that cause an allergic reaction and inflammation.
Here I only found a single publication linking mast cells to tendon damage (8). This paper theorizes that the neurologic inflammation that can be triggered by mast cells could theoretically damage tendons. However, it draws no direct link between the two. This is again, tendon damage and NOT ligament damage.
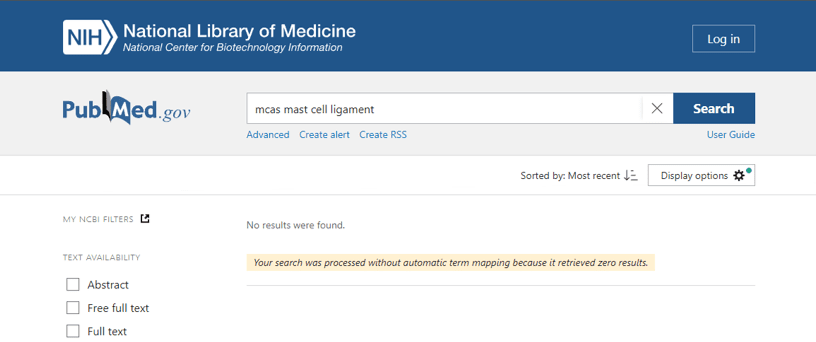
I didn’t find anything else listed as involving MCAS and ligament damage:
BOTTOM LINE: We have no scientific research linking MCAS to ligament damage.
Diet
There are a few concepts in this category:
- Dietary trigger
- Chemicals replacing sulfur in collagen molecules
- Gut dysbiosis
Dietary Trigger
The idea here is similar to the scenario above. A dietary trigger like gluten leads to chronic inflammation and this causes ligament damage. However, even if we consider the more severe version of gluten sensitivity called celiac disease which involves wasting and causes severe illness, I can find no research connecting gluten exposure to ligament damage.
BOTTOM LINE: We have no scientific research linking Gluten to ligament damage.
Chemicals Replacing Sulfur in Collagen Molecules
This is an interesting theory that begins usually with yeast overgrowth or dysbiosis in the gut producing a chemical called oxalates. The theory is that these oxalates will replace sulfur molecules in collagen which will weaken the structure of that ligament building block. However, nothing applicable to oxalates actually damaging ligaments is found when searching the US National Library of Medicine:
BOTTOM LINE: We have no scientific research linking oxalates replacing sulfur in collagen molecules to ligament damage.
Gut Dysbiosis/Microbiome/SBIO
Another theory is that the microbiome in your gut could be linked to ligament damage. This goes by a few names like gut dysbiosis or SBIO (Small Intestine Bacterial Overgrowth). While there is little evidence that any of these issues have anything to do with ligaments, there is some interesting real scientific research in this area involving arthritis and pain.
For example:
- An interesting scientific review that tries to link disorders of the gut microbiome to arthritis. (9)
- Mice fed a high-fat diet developed what we would call “metabolic syndrome” had higher systemic inflammation and developed knee arthritis. (10) Giving them pre-biotics (oligofructose) helped the gut bacteria composition and the bad inflammation.
- Back pain was associated with an abnormal gut microbiome, likely due to what we would call “metabolic syndrome”. (11)
Despite this promising research, I could find no link between things like SBIO and ligament damage.
BOTTOM LINE: We have no scientific research linking your gut microbiome to ligament damage. There is some emerging evidence linking your gut microbiome to arthritis and perhaps spine pain, so it’s not inconceivable that other connections could be discovered.
Chronic Inflammation
One of the most common afflictions of industrialized, first-world societies is chronic low-grade inflammation. That usually comes from metabolic syndrome which is defined as:
- Overweight
- High blood pressure
- High triglycerides
- Insulin resistance (pre-diabetes)
There is some interesting research in this area around this type of damaging inflammation and tendon problems, but not about ligament laxity or damage:
- Mice that were given an allergen to cause chronic inflammation show weaker tendons and people with allergies show more signs of tendinopathy (12).
- Normal tendon healing is adversely impacted by low-level inflammation. (13)
- It’s thought that patients with high MMP-9 levels (a marker for low-grade inflammation) may be more likely to have age-related tendon problems. (14)
Given that metabolic syndrome is common here in the US, we have long recommended some common sense things to do when considering an orthobiologics procedure:
- Clean up your diet to reduce chronic inflammation associated with metabolic syndrome.
- Lose weight to reduce the effects of metabolic syndrome.
- Improve sleep
- Take anti-inflammatory supplements that have been shown via randomized controlled trials to reduce chronic inflammation.
On losing weight, see this blog. On eating right, see Dr. Pitts’ book:
BOTTOM LINE: We know that chronic inflammation is a killer that impacts your joints and tendons. We don’t have research showing that it hurts your ligaments directly, but cleaning this up is an important part of conquering chronic pain.
The upshot? We don’t really have lots of research connecting these common functional medicine diagnoses to ligament damage. However, that doesn’t mean that some may not be discovered. In the meantime, of the above list of things that could be tied to ligament and musculoskeletal issues, the most research exists for gut dysbiosis and metabolic syndrome which go hand in hand. The good news is that those are things that are easier to control.
_________________________________________
(1) Tabar MD, Tabar J, Naranjo C, Altet L, Roura X. Detection of vector-borne pathogens in owned dogs with cranial cruciate ligament rupture living in the Mediterranean area. Parasit Vectors. 2022 May 10;15(1):105. doi: 10.1186/s13071-022-05205-x. PMID: 35534857; PMCID: PMC9088045.
(2) Häupl T, Hahn G, Rittig M, Krause A, Schoerner C, Schönherr U, Kalden JR, Burmester GR. Persistence of Borrelia burgdorferi in ligamentous tissue from a patient with chronic Lyme borreliosis. Arthritis Rheum. 1993 Nov;36(11):1621-6. doi: 10.1002/art.1780361118. PMID: 8240439.
(3) Müller KE. Erkrankungen der elastischen und kollagenen Fasern von Haut, Sehnen und Bänder bei Lyme-Borreliose. umwelt-medizin-gesellschaft. 2009;22(2):112–8.
(4) Muir P, Oldenhoff WE, Hudson AP, Manley PA, Schaefer SL, Markel MD, Hao Z. Detection of DNA from a range of bacterial species in the knee joints of dogs with inflammatory knee arthritis and associated degenerative anterior cruciate ligament rupture. Microb Pathog. 2007 Feb-Mar;42(2-3):47-55. doi: 10.1016/j.micpath.2006.10.002. Epub 2007 Feb 21. PMID: 17320342.
(5) Omar IM, Weaver JS, Samet JD, Serhal AM, Mar WA, Taljanovic MS. Musculoskeletal Manifestations of COVID-19: Currently Described Clinical Symptoms and Multimodality Imaging Findings. Radiographics. 2022 Sep-Oct;42(5):1415-1432. doi: 10.1148/rg.220036. Epub 2022 Jul 22. PMID: 35867593; PMCID: PMC9341171.
(6) Khoja O, Silva Passadouro B, Mulvey M, Delis I, Astill S, Tan AL, Sivan M. Clinical Characteristics and Mechanisms of Musculoskeletal Pain in Long COVID. J Pain Res. 2022 Jun 17;15:1729-1748. doi: 10.2147/JPR.S365026. PMID: 35747600; PMCID: PMC9212788.
(7) Valent P, Akin C, Nedoszytko B, Bonadonna P, Hartmann K, Niedoszytko M, Brockow K, Siebenhaar F, Triggiani M, Arock M, Romantowski J, Górska A, Schwartz LB, Metcalfe DD. Diagnosis, Classification and Management of Mast Cell Activation Syndromes (MCAS) in the Era of Personalized Medicine. Int J Mol Sci. 2020 Nov 27;21(23):9030. doi: 10.3390/ijms21239030. PMID: 33261124; PMCID: PMC7731385.
(8) Alim MA, Peterson M, Pejler G. Do Mast Cells Have a Role in Tendon Healing and Inflammation? Cells. 2020 May 4;9(5):1134. doi: 10.3390/cells9051134. PMID: 32375419; PMCID: PMC7290807.
(9) Berthelot J, Sellam J, Maugars Y, et alCartilage-gut-microbiome axis: a new paradigm for novel therapeutic opportunities in osteoarthritisRMD Open 2019;5:e001037. doi: 10.1136/rmdopen-2019-001037
(10) Schott EM, Farnsworth CW, Grier A, Lillis JA, Soniwala S, Dadourian GH, Bell RD, Doolittle ML, Villani DA, Awad H, Ketz JP, Kamal F, Ackert-Bicknell C, Ashton JM, Gill SR, Mooney RA, Zuscik MJ. Targeting the gut microbiome to treat the osteoarthritis of obesity. JCI Insight. 2018 Apr 19;3(8):e95997. doi: 10.1172/jci.insight.95997. PMID: 29669931; PMCID: PMC5931133.
(11) Dekker Nitert M, Mousa A, Barrett HL, Naderpoor N, de Courten B. Altered Gut Microbiota Composition Is Associated With Back Pain in Overweight and Obese Individuals. Front Endocrinol (Lausanne). 2020 Sep 2;11:605. doi: 10.3389/fendo.2020.00605. PMID: 32982987; PMCID: PMC7492308.
(12) Lehner C, Spitzer G, Langthaler P, Jakubecova D, Klein B, Weissenbacher N, Wagner A, Gehwolf R, Trinka E, Iglseder B, Paulweber B, Aigner L, Couillard-Després S, Weiss R, Tempfer H, Traweger A. Allergy-induced systemic inflammation impairs tendon quality. EBioMedicine. 2022 Jan;75:103778. doi: 10.1016/j.ebiom.2021.103778. Epub 2022 Jan 7. PMID: 35007819; PMCID: PMC8749446.
(13) Chisari E, Rehak L, Khan WS, Maffulli N. Tendon healing is adversely affected by low-grade inflammation. J Orthop Surg Res. 2021 Dec 4;16(1):700. doi: 10.1186/s13018-021-02811-w. PMID: 34863223; PMCID: PMC8642928.
(14) Gonçalves FM, Jacob-Ferreira AL, Gomes VA, Casella-Filho A, Chagas AC, Marcaccini AM, Gerlach RF, Tanus-Santos JE. Increased circulating levels of matrix metalloproteinase (MMP)-8, MMP-9, and pro-inflammatory markers in patients with metabolic syndrome. Clin Chim Acta. 2009 May;403(1-2):173-7. doi: 10.1016/j.cca.2009.02.013. Epub 2009 Feb 28. PMID: 19254704.
Original Article: https://regenexx.com/blog/can-things-like-lyme-mold-or-covid-or-your-diet-destroy-your-ligaments/
.png)
.png)







Comments
Post a Comment