Some doctors and media channels argue that there is very little evidence to
support the use of dietary supplements to prevent or treat COVID-19. However,
as of September 2021, there are
more than 60 publications related to dietary supplements and COVID-19.
There are more than 80 types of supplements that are being studied for
COVID-19. Vitamin D remains the most studied vitamin with the most evidence followed
by zinc and vitamin C, for COVID-19. You can review the details of these
trials on
clinicaltrials.gov.
This guide is based on various references to scientific literature and
hopefully, can help you make sense of the options and to separate the facts
from fiction.
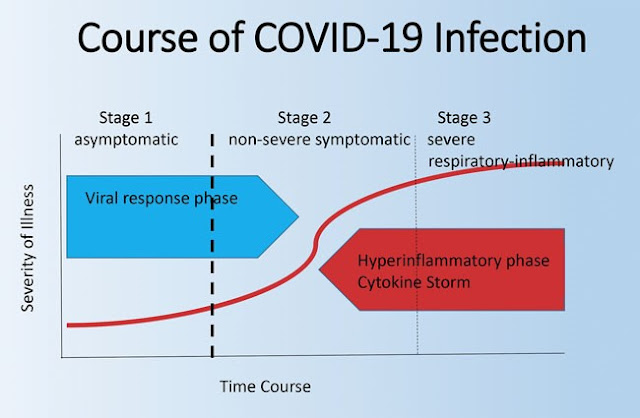
Image credit: ClevelandClinic
Note: This is a highly dynamic topic; therefore, we will be updating
this article as new information or evidence emerges.
Contents
- Vitamin D3
- Quercetin
- Vitamin C
- Zinc
- Curcumin and Turmeric
- Melatonin
- NAC and Glutathione
- Omega 3 (Fish Oil)
- Selenium
- B Vitamins
- Molecular Hydrogen
- Lactoferrin
- Probiotics
- Green Tea (EGCG)
- Astaxanthin
1. Vitamin D3
Vitamin D, whose forms are vitamin D2 and vitamin D3, is an essential
nutrient that is naturally present in only a few foods, such as fatty fish
(including salmon and tuna), fish liver oils, beef liver, cheese, and egg
yolks. Fortified foods, especially fortified milk, provide most of the
vitamin D in American diets. The
RDA
for vitamin D ranges from 10 to 15 mcg (400 international units [IU] to
600 IU) for children (depending on age) and from 15 to 20 mcg (600 to 800
IU) for adults. The body can also synthesize vitamin D from sun exposure.
Vitamin D obtained from sun exposure, foods, and supplements is
biologically inert and must undergo two transformations in the body for
activation. The first transformation, which occurs in the liver, converts
vitamin D to 25-hydroxyvitamin D [25(OH)D]. The second transformation
occurs primarily in the kidney and forms the physiologically active
1,25-dihydroxyvitamin D [1,25(OH)2D]. Serum concentration of 25(OH)D is
currently the main indicator of vitamin D status. Although
researchers have not definitively identified serum concentrations of
25(OH)D associated with deficiency and adequacy, the FNB advises that
levels below 30 nmol/L (12 ng/mL) are associated with vitamin D
deficiency, and levels of 50 nmol/L (20 ng/mL) or more are considered
adequate for bone and overall health in most people [
Source].
In addition to its well-known effects on calcium absorption and bone
health, vitamin D plays a role in immunity [
Source]. Vitamin D appears to lower viral replication rates,
suppress inflammation, and increase levels of T-regulatory cells and their
activity. In addition, immune cells (e.g., B lymphocytes and T
lymphocytes) express the vitamin D receptor and some immune cells (e.g.,
macrophages and dendritic cells) can convert 25(OH)D into the active
1,25(OH)2D. This ability suggests that vitamin D might modulate immune
responses.
Vitamin D deficiency affects the body’s susceptibility to infection and has
been associated with influenza, hepatitis C, human immunodeficiency virus
(HIV) and other viral diseases [
Source]. Surveys indicate that most people in the United States consume less than
recommended amounts of vitamin D. Nevertheless, according to a 2011–2014
analysis of serum 25(OH)D concentrations, most people in the United States
aged 1 year and older had adequate vitamin D status. Sun exposure, which
increases serum 25(OH)D levels, is one of the reasons serum 25(OH)D levels
are usually higher than would be predicted on the basis of dietary vitamin D
intakes alone.
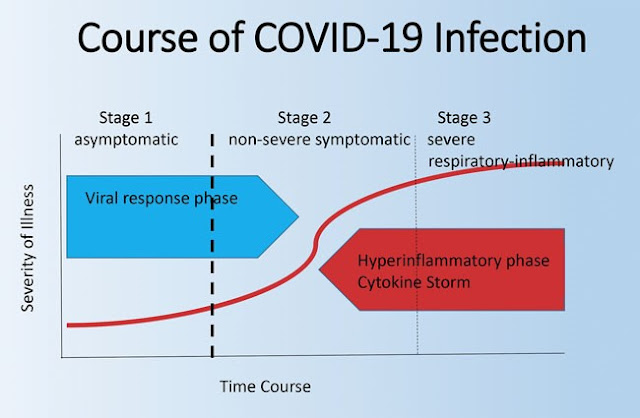
Vitamin D and COVID-19
Based on several publications and studies,
vitamin D seems to be the “most promising” natural supplement for COVID-19
protection. Vitamin D deficiency is known to enhance a process known as
the “cytokine storm” (
Marik, Jun 2020).
In a study (
Frontiers in Immunology, Dec 2020) using bioinformatics and systems biology approach, the pathways
associated with cytokine storm in COVID-19 is identified and suggested
that the underlying mechanism of vitamin D could be promising in
suppressing the cytokine storm.
Trusted Source).
In a study from Nature (
Sci Rep, May 2021) to investigate the effects of daily high-dose supplementation (60,000
IUs) of vitamin D — for eight to 10 days, in addition to standard therapy,
for COVID-19 patients deficient in vitamin D; Vitamin D levels increased
significantly in the vitamin D group — from 16 ng/ml to 89 ng/ml — while
inflammatory markers significantly decreased, without any side effects.
The largest
observational study to date, looked at data for 191,779 American patients who were
tested for SARS-CoV-2 between March and June 2020 and had had their
vitamin D tested sometime in the preceding 12 months.
Of
those with a vitamin D level below 20 ng/ml (deficiency), 12.5% tested
positive for SARS-CoV-2, compared to 8.1% of those who had a vitamin D
level between 30 and 34 ng/ml (adequacy) and 5.9% of those who had an
optimal vitamin D level of 55 ng/ml or higher.
Data from
14 observational studies — suggest that vitamin D blood levels are negatively correlated
with the incidence and/or severity of COVID-19; meaning if your vitamin
D level is high, your risk for COVID-19 is low and vice versa.
A study published in November 2020 from Singapore (
CW Tan, Nutrition 2020), found that those who were started on a daily oral dose of
vitamin D3 (1,000 IU), magnesium (150 mg) and vitamin B12 (500 mcg)
within the first day of hospitalisation and continued up to 14 days
were significantly less likely to require oxygen therapy and further
intensive care.
According to the statement
released on 2 October 2020 by the U.S. president’s physician said that in addition to
the antibodies, Trump “has been taking zinc, vitamin D, famotidine,
melatonin and a daily aspirin.”
Another study, published in JAMA (
JAMA Netw Open - Sep 2020) found that persons who are likely to have deficient vitamin D
levels at the time of COVID-19 testing were at substantially
higher risk of testing positive for COVID-19 than were persons who
were likely to have sufficient levels.
A
study of 20 European countries found a link between low levels of
vitamin D and higher percentages of COVID-19 cases and mortality.
Separately, more than 80% of 200 people hospitalized for COVID-19
in Spain were found to be deficient in vitamin D, according to
a
study published in October 2020 in the Journal of Clinical
Endocrinology & Metabolism.
A review by Dinicolantonio et al (
Mo Med Feb 2021) also suggested vitamin D and magnesium deficiency as a
potential cause of cytokine storm in COVID-19 patients and
recommended that vitamin D and magnesium supplementation to be
considered.
There are many vitamin D studies underway. You can review the status
of these trials on
clinicaltrials.gov. As of July 2021, more than 40 studies have been launched to
investigate the benefits of vitamin D against COVID-19.
Check out the evidence tracker on vitamin D and COVID-19 from
c19vitamind.com (constantly updated).
Safety: Daily intakes of up to
25–100 mcg (1,000 IU–4,000 IU)
vitamin D in foods and dietary supplements are safe for children (depending
on their age) and up to 100 mcg (4,000 IU) are safe for adults. These
values, however, do not apply to individuals receiving vitamin D treatment
under the care of a physician. Higher intakes (usually from supplements) can
lead to nausea, vomiting, muscle weakness, confusion, pain, loss of
appetite, dehydration, excessive urination and thirst, and kidney stones. In
extreme cases, vitamin D toxicity causes renal failure, calcification of
soft tissues throughout the body (including in coronary vessels and heart
valves), cardiac arrhythmias, and even death.
2. Quercetin
Quercetin is a pigment that is found in plants, vegetables, and fruits, and
serves as an immune nutrient offering many health benefits. Elderberry, red
onions, white onions and cranberries are the richest sources of quercetin.
It is a flavonoid and antioxidant that may help to reduce inflammatory
cytokines, infections, allergies and
anti-blood clot property. Research has found that quercetin may be particularly beneficial for
viral respiratory infections.
Quercetin and COVID-19
An Italo-Pakistani, randomized trial of Quercetin (
Di Pierro et al 2021) in high bioavailability form in Covid outpatients (n=152) yields
spectacular results that beg for immediate reproduction: > 68% less
hospitalizations, which are 78% shorter and 100% less ICU admissions or
deaths.
As of September 2021, more than 10
studies have been launched to investigate the benefits of quercetin against COVID-19.
Ultimately, the results of the above trials will offer more definitive
evidence.
Quercetin
was initially found to provide broad-spectrum protection against SARS coronavirus in
the aftermath of the SARS epidemic that broke out across 26 countries in
2003. Now, some doctors are advocating its use against SARS-CoV-2, in
combination with vitamin C, noting that the two have synergistic
effects.
Quercetin, Vitamin C, D, Zinc and Melatonin - FLCCC I-MASK+
Protocol
Incidentally, ascorbic acid (
vitamin C) and the bioflavonoid quercetin (originally labeled vitamin P) were both discovered by the same scientist — Nobel prize winner
Albert Szent-Györgyi. Quercetin and vitamin C also act as an antiviral drug, effectively inactivating viruses.
There is evidence that vitamin C and quercetin co-administration exerts a synergistic antiviral action due to overlapping antiviral and immuno-modulatory properties and the capacity of ascorbate to recycle quercetin, increasing its efficacy.
For updated prevention and early outpatient protocol for COVID-19 positive, please check out FLCCC I-MASK+ protocol.
Quercetin, Zinc, Vitamin D and C: AAPS (Association of American
Physicians and Surgeons) Guidelines
The AAPS recommends the following outpatient nutraceutical 'treatment'
protocol for COVID-19:
-
Quercetin oral 500 mg twice a day (Amazon)
-
Vitamin C 3000 mg (Amazon)
-
Vitamin D3 5000 IU (Amazon)
-
Zinc sulphate 220 mg (equivalent to 50 mg of elemental zinc) (Amazon)
Please take note the above dosages are relatively high and is meant for
'treatment'. If you wish to continue taking these nutrients for health
maintenance, you'll need to reduce the dosages based on the recommended
dietary allowance (RDA or RDI) after you've recovered.
A word about quercetin: Some physicians are recommending this supplement
to reduce viral illnesses because quercetin acts as a zinc ionophore to
improve zinc uptake into cells. It is much less potent than HCQ
(hydroxychloroquine) as a zinc transporter, and it does not reach high
concentrations in lung cells that HCQ does. Quercetin may help reduce risk
of viral illness if you are basically healthy. But it is not potent enough
to replace HCQ for treatment of COVID once you have symptoms, and it does
not adequately get into lung tissue unless you take massive doses (3-5
grams a day), which cause significant GI (gastrointestinal) side effects
such as diarrhea.
3. Vitamin C
Vitamin C may be one of the most well-known immune nutrients that protect
against immune deficiencies and which supports the prevention and recovery
from the common cold and upper-respiratory issues, and also protects your
cardiovascular system, eyes, skin, and other parts of your body. Research
has found that vitamin C may help to optimize the immune system.
Vitamin C and COVID-19
There are many vitamin C studies underway and you can review the
status of these trials on
clinicaltrials.gov. As of July 2021, there are more than 20 studies that have been
launched to investigate the benefits of vitamin C against COVID-19.
Most people turn to vitamin C after they've caught a cold. That’s
because it helps build up your immune system. Vitamin C is thought to
increase the production of white blood cells. These are key to fighting
infections. Some of the most vitamin C-rich foods include citrus fruits,
from tangerines to limes, along with leafy greens, bell peppers, papaya
and broccoli. Berries are another great source, and they all provide
this and other potent antioxidants, which support your immune response
and help to rebuild collagen. Because your body doesn't produce or store
it, you need daily vitamin C for continued health. Almost all citrus
fruits are high in vitamin C.
Vitamin C might help prevent COVID-19 and also lessen the inflammatory
reactions behind some severe COVID-19 cases, according to a
review of research on the topic published in the latest issue of the journal Nutrition.
Check out the evidence tracker on vitamin C and COVID-19 from
c19vitaminc.com (constantly updated).
The U.S. Recommended Dietary Allowance (RDA) for vitamin C is 75 to 120
milligrams per day.
Safety: Taking large doses of vitamin C (ascorbic
acid) on a regular basis lowers your level of copper, so if you are
already deficient in copper and take high doses of vitamin C, you can
compromise your immune system.
While generally considered safe even in high doses, way too much vitamin
C — anything above 2,000 milligrams daily—can cause headaches, insomnia,
diarrhea, heartburn, and other issues.
Temporarily taking megadoses of vitamin C supplements to combat a
case of the cold or flu is likely not going to cause a problem.
Many vitamin C supplements that are above the US RDA are sold in the
market. It’s important to seek a physician’s advice if you intend to take
high dose vitamin C on a long term basis. To be on the safe side, you may
also request for your kidney functions to be monitored.
For long-term, daily use, your best bet is to eat a diet that is full of
high quality organic vegetables and fruits that are minimally processed.
Not only will you get vitamin C, but you will get all the other accessory
nutrients and micronutrients that are needed to optimize it.
4. Zinc
Zinc is another powerful immune nutrient known for its benefits for
providing immune health support and inflammation reduction as well as
for improving cold and respiratory symptoms, wound healing, acne
reduction, and lowering the risk of age-related diseases. Research on
atherosclerosis and diabetes mellitus suggests that zinc deficiency may
contribute to low-grade systemic inflammation.
Aging is associated with compromised immunity, that just means that your
immune response to pathogens and infections starts to slow and is less
robust, including a reduced vaccine immune response/efficacy.
Improving
zinc intake/zinc status improves/modulates/enhances immune
function. The flip side is, while some aspects of immunity slow,
others increase. Uncontrolled immune responses drive excess
inflammation. Zinc helps to balance all of this.
Zinc and COVID-19
A retrospective study (
Carlucci et al, Oct 2020) analyzed outcomes in 411 patients hospitalized with an acute viral
respiratory infection who were treated with 440 mg of zinc sulfate
(providing 100 mg of elemental zinc) daily for five days in addition to
hydroxychloroquine and azithromycin. When these patients’ outcomes were
compared with those of 521 similar patients who received the same
treatment but without zinc, those who received zinc were more likely to
have been discharged home and, among those who did not require intensive
care, the individuals given zinc were less likely to die or be transferred
to hospice care than those who received no zinc.
Interestingly, some researchers have proposed low zinc status may
contribute to the loss of smell that sometimes accompanies respiratory
viral infections (
J Clin Biochem Nutr. 2021 Jan); while one study found no significant relationship between zinc status
and loss of smell in 134 patients with a viral respiratory infection, it
did note those who received 50 mg elemental zinc twice daily recovered
their sense of smell more quickly than those who received no zinc (
Abdelmaksoud et al. 2021 Jan).
There are many Zinc studies underway and you can review the status of
these trials on
clinicaltrials.gov. As of April 2021, there are more than 20 studies that have been
launched to investigate the benefits of Zinc against COVID-19.
Foods that are high in zinc include oysters, crab, lobster, mussels, red
meat, and poultry. Cereals are often fortified with zinc. Most
multivitamin and nutritional supplements contain zinc.
Zinc has been shown in a lab study to inhibit regular coronavirus (not
the current SARS-CoV-2) since 2010, in a
2010 publication.
Check out the evidence tracker on zinc and COVID-19 from
c19zinc.com (constantly updated).
Safety: Taking zinc long term is typically safe for healthy
adults, as long as the daily dose is under the set upper limit of 40
mg of elemental zinc (
PubMed). Be aware that typical daily doses of zinc provided by zinc lozenges
generally exceed tolerable upper limits for zinc, and for this reason,
they
should not be used for longer than about a week.
Excessive doses may interfere with copper absorption, which
could negatively affect your immune system as it
can cause copper deficiencies, blood disorders and potentially permanent nerve damage. Zinc can
also impair the absorption of antibiotics, and use of zinc nasal gels
or swabs has been linked to temporary or permanent loss of smell.
The ideal dose for prevention while the COVID-19 risk is high is
40-100 mg/d, a portion of which comes from zinc lozenges to spread
the zinc through the tissues of the nose, mouth and throat. It
should be accompanied by at least 1 mg copper from food and
supplements for every 15 mg zinc.
Do take note that you should keep the dosage back to within 40
mg/d once the exposure risk is back to normal.
5. Curcumin and Turmeric
Curcumin, a yellow carotenoid from turmeric, is well known for its
anti-inflammatory and free radical-scavenging effects.
Curcumin and COVID-19
There are
4 studies of curcumin in COVID-19 published, including 3 double-blind
randomized controlled trials and 1 review. And the results are promising.
It has also demonstrated antiviral effects against a range of respiratory
viruses, including influenza A virus and others (
Ref). Computer models suggest curcumin may interfere with viral entry into
cells as well as viral replication inside cells (
Ref). Numerous preclinical studies indicate curcumin may activate antiviral
immunity; at the same time, curcumin appears to inhibit infection-induced
inflammatory signaling and promote anti-inflammatory processes, reducing
the potential for a cytokine storm and ARDS and protecting other organ
systems (
Ref). By suppressing inflammation, curcumin has the potential to help
mitigate complications and sequelae of severe acute viral respiratory
infections (
Ref).
Curcumin has been demonstrated (
Ref) to suppress several inflammatory cytokines and mediators of their
release such as tumor necrosis factor-alpha (TNF-alpha), IL-1, IL-8 and
nitric oxide synthase.
In an open-label trial, 21 patients
hospitalized with mild-to-moderate illness due to a highly infectious
respiratory virus were treated with a nano-curcumin preparation providing
80 mg curcuminoids (curcumin and its related compounds) twice daily for
two weeks in conjunction with standard therapies; their progress was
compared with 20 similar patients treated with standard therapies alone.
Those who received curcumin had better oxygenation status beginning on day
two of treatment, as well as faster resolution of most symptoms, faster
normalization of immune cell numbers, less likelihood of worsening of
their clinical status, shorter time requiring supplemental oxygen, and
shorter hospital stays (
Ref).
In a double-blind placebo-controlled trial of 40
participants with a viral respiratory illness, those who received 160 mg
nano-curcumin per day for 14 days along with standard therapy had greater
reductions in some inflammatory cytokines, including IL-6. They also
experienced significant improvement in more symptoms and had a lower
fatality rate than those receiving placebo (
Ref).
The same research group conducted another double-blind placebo-controlled
trial in hospitalized patients with the same virulent respiratory virus,
40 with severe illness receiving intensive care and 40 with mild illness;
half of the participants in each group received 160 mg nano-curcumin per
day for 14 days and the other half received placebo. Curcumin-treated
patients had lower numbers and activity of immune cells known to be
involved in cytokine storm and hyper-inflammation. They also had greater
improvement in fever, cough, and shortness of breath, and had lower
mortality rates (0% vs. 5% in those with mild illness and 5% vs. 25% in
those with severe illness [p<.0001 for both mild and severe cases])
than those who received placebo (
Ref).
6. Melatonin
Melatonin is a hormone produced by the pineal gland in the brain, mainly
during the night, that helps regulate circadian rhythms [
Source]. Its levels decrease with aging. Most melatonin supplementation
studies have evaluated its ability to control sleep and wake cycles,
promote sleep, and reduce jet lag.
Laboratory and animal
studies suggest that melatonin enhances immune response by increasing
the proliferation and maturation of natural killer cells, T and B
lymphocytes, granulocytes and monocytes . Melatonin also appears to have
anti-inflammatory and antioxidant effects [
Source]. However, whether these properties have a clinically significant
effect on immunity in humans is not clear.
Melatonin and COVID-19
The potential utility of melatonin in treating COVID patients has not
gone unnoticed, with a PubMed search combining melatonin and COVID
producing more than 50 citations.
Assisting sleep and rest is already an immune system-supporting benefit,
but melatonin has more to offer. It is a powerful antioxidant that
supports your immune health, brain, eyes, digestion, and more. It may
even be helpful when it comes to COVID-19.
Melatonin is a hormone synthesized in your pineal gland and many
other organs. While it is most well-known as a natural sleep
regulator, it also has many other important functions. For example,
melatonin is a potent antioxidant (
Antioxidants, 2020) with the rare ability to enter your mitochondria, where it helps
“prevent mitochondrial impairment, energy failure and apoptosis of
mitochondria damaged by oxidation.” It also helps recharge
glutathione and
glutathione deficiency has been linked to COVID-19 severity.
As discussed in a review (
Cardinali et al. 2020), melatonin might counteract the consequences of COVID-19 via salutary effects on the sleep/wake cycle and more generally on chronobiology, as well as through its antioxidant and anti-inflammatory effects.
Based on melatonin’s therapeutic potential and well-established
safety profile, it has been suggested those at higher risk for
severe illness and complications from viral respiratory infection,
including the elderly and those with chronic medical conditions, may
benefit most from regular use of 3–10 mg melatonin at bedtime (
Ref).
Fluvoxamine (Selective Serotonin Reuptake Inhibitor) might also exert
beneficial effects in COVID patients through its
well-characterized ability to substantially increase (~ 2–3-fold)
night-time plasma levels of melatonin. This increase appears to
result from fluvoxamine’s inhibition of the melatonin-metabolizing
liver enzymes (
von Bahr et al. 2000.
An
Iranian randomised controlled trial (Arch Med Res 2021), studied 74 mild to moderate
hospitalized patients. The study showed that adjuvant use of
melatonin has a potential to improve clinical symptoms of COVID-19
patients and contribute to a faster return of patients to baseline
health.
Data from Cleveland Clinic supports the use of melatonin. Here, the researchers analyzed
patient data from the Cleveland Clinic’s COVID-19 registry using an
artificial intelligence platform designed to identify drugs that may
be repurposed.
"Patients who used melatonin as a supplement had, on average, a 28%
lower risk of testing positive for SARS-CoV-2. Blacks who used
melatonin were 52% less likely to test positive for the virus."
Some researchers have suggested high doses of melatonin, ranging from
50 to 200 mg twice daily, might help treat patients hospitalized for
severe acute respiratory illness (
Ref).
In a small
Philippine case series study of 10 hospitalised COVID-19 patients, high dose
melatonin (hdM) was given in addition (adjuvant) to standard
therapy. According to the authors:
"High dose melatonin may have a beneficial role in patients
treated for COVID19 pneumonia, in terms of shorter time to
clinical improvement, less need for MV, shorter hospital stay, and
possibly lower mortality."
Production of melatonin diminishes with age, contributing to immune
dysfunction and increasing oxidative stress, inflammation, and infection
susceptibility (
Ref). In addition, infectious viruses can suppress melatonin production,
disrupting circadian controls and impairing immune function (
Ref).
Melatonin supplementation may reduce the risk of acute
viral respiratory infections, help mitigate some chronic health problems
that increase infection vulnerability, and protect against neurological
and cardiovascular complications of viral respiratory infections (
Reiter et al. 2020).
One study found that among 26,779 people tested for COVID-19, those who
reported using melatonin supplements were less likely to have the
disease (
PLoS Biol. 2020).
In another observational study that followed 11,672 individuals,
melatonin use was associated with a reduced risk of testing positive for
a common, highly infectious respiratory virus (
Ref).
Another study looked at data from 791 patients intubated for respiratory
support during an outbreak of a severe acute viral respiratory illness
and 2,981 patients needing the same level of respiratory support for
other reasons. The use of melatonin, most often for sleep issues, during
the intubation period was associated with significantly improved
outcomes in both groups and increased the likelihood of survival in
virus-infected patients who required mechanical ventilation (
Ref).
As of July 2021, more than 8
studies are currently underway to investigate the benefits of melatonin against COVID-19.
Ultimately, the results of the above trials will offer more definitive
evidence.
Safety: If you take a melatonin supplement, be
careful:
Too much can cause daytime sleepiness. There is no federal RDA nor any formal advice on supplement dose
ranges. Based on an on-going
Spanish study, a 2 mg daily dose protocol is being investigated for prevention of
COVID-19. Do take note that the dosage for 'prevention' and 'treatment' is
different, For prevention or maintenance, a lower dosage is normally
recommended whereas a 'treatment' or 'therapeutic' dosage is normally
higher.
Typical doses of 1–10 mg/day melatonin appear to be safe for short-term
use (
Source). Reported side effects, which are usually minor, include dizziness,
headache, nausea, upset stomach, rash, and sleepiness. However, some
reports have linked high blood levels of melatonin with delayed puberty
and hypogonadism.
Studies have not evaluated melatonin
supplementation during pregnancy and breastfeeding, but some research
suggests that these supplements might inhibit ovarian function (
Source). Therefore, some experts recommend that women who are pregnant or
breastfeeding avoid taking melatonin.
Related: Nature's Bounty Melatonin 5 mg > One tablet before
bedtime (Amazon)
N-acetylcysteine (NAC) is a precursor to glutathione. It is an
antioxidant and increases glutathione levels in the body (
Source). NAC has mucolytic activity, so it helps reduce respiratory
mucus levels. Laboratory research suggests that NAC might boost
immune system function and suppress viral replication. NAC also
decreases levels of interleukin-6 and has other anti-inflammatory
effects.
Much of the research on NAC has used an inhaled, liquid form of
this compound. This form—which is classified as a drug, not a dietary
supplement—is approved by the U.S. Food and Drug Administration (FDA)
as a mucolytic agent and for decreasing respiratory secretion
viscosity (
Source). Products containing NAC are also sold as dietary supplements.
NAC and COVID-19
According to this
paper (2021), SARS-CoV2 infection impairs the metabolism and redox
function of cellular glutathione. According to the authors, NAC can
prevent this damage and the role of NAC in COVID-19 therapy is worth
investigating.
Studies published in ACS Infectious Disease (
ACS Infect Dis. 2020) and
Antioxidants proposed that glutathione plays a crucial role in the
body's fight against the severe inflammatory response triggered by
the SARS-CoV-2 virus. The research group in the ACS Infectious
Disease study called it the “most likely cause of serious
manifestations and deaths in COVID-19 patients.”
NAC inhibits cellular entry and replication of some respiratory
viruses, assists in clearing thickened mucous from the airways,
suppresses inflammatory signaling, and may help mitigate viral
infection-induced cytokine storm (
Ref).
In a paper on NAC for COVID-19, published in
the
October 2020 issue of Clinical Immunology titled “Therapeutic Blockade of Inflammation in Severe
COVID-19 Infection With Intravenous N-acetylcysteine”, which is
a case series report of 10 patients (including one with G6PD
deficiency) given intravenous NAC. NAC elicited clinical
improvement and markedly reduced inflammatory marker, CRP in all
patients. NAC mechanism of action may involve the blockade of
viral infection and the ensuing cytokine storm.
Another study, "Endogenous Deficiency of Glutathione as the Most
Likely Cause of Serious Manifestations and Death in COVID-19
Patients" was led by Dr Alexey Polonikov from Russia (
ACS Infect Dis. 2020).
What he found was that the
reactive-oxygen-species-to-glutathione ratio was able to
predict the severity of COVID-19 and the patient’s outcome.
When the patient had a low ROS-to-glutathione ratio, the
patient had a very mild case. The fever disappeared on the
fourth day without any treatment whatsoever.
When the ROS-to-glutathione ratio was high, the
patient developed air hunger on the fourth day, experienced
significant fever, hoarseness, myalgia and fatigue
persisting for 13 days. A patient with even higher ROS and
lower reduced glutathione had critical disease requiring
hospitalisation for COVID-19-related pneumonia.
In another
publication on Respiratory Medicine Case Reports:
Two patients living in New York City (NYC) with a
history of Lyme and tick-borne co-infections
experienced a cough and dyspnea and demonstrated
radiological findings consistent with novel
coronavirus pneumonia (NCP). A trial of 2 g of PO or
IV glutathione was used in both patients and improved
their dyspnea within 1 h of use. Repeated use of both
2000 mg of PO and IV glutathione was effective in
further relieving respiratory symptoms.
Foods that have a positive impact on glutathione
production include cruciferous vegetables such as
broccoli, green tea, curcumin, rosemary and milk thistle.
Getting quality sleep may also help.
Different
types of exercise can influence your levels as well.
In
one study, researchers enrolled 80 healthy but sedentary
volunteers to measure the type of exercise that may have
the greatest effect. They found that aerobic training in
combination with circuit weight training showed the
greatest benefit.
As of July 2021, more than 10
clinical trials are underway to assess the efficacy of NAC in the context
of highly infectious respiratory viral infections.
What Is the Primary Cause of Severe COVID-19 Illness:
Glutathione or Vitamin D Deficiency?
The hypothesis that vitamin D (VD) deficiency is responsible for
severe manifestations and death in COVID-19 patients has been
proposed and is actively being discussed by the scientific
community.
Several studies reported that glutathione levels positively
correlate with active vitamin D. (
PubMed,
PubMed)
Interestingly, a recent experimental study (
PubMed) showed that Glutathione deficiency and the associated
increased oxidative stress epigenetically alters vitamin D
regulatory genes and, as a result, the suppressed gene
expression decreases Vitamin D production, ultimately leading to
a secondary deficiency of vitamin D. This study provides
important information that glutathione is essential for the
control of endogenous vitamin D production and demonstrates
potential benefits of Glutathione treatment in reducing the
deficiency of vitamin D. Taken together, these findings suggest
that glutathione deficiency rather than vitamin D deficiency is
a primary cause underlying biochemical abnormalities, including
the decreased biosynthesis of vitamin D, and is responsible for
serious manifestations and death in COVID-19 patients.
NAC (N-Acetyl Cysteine) vs Glutathione
N-acetyl L-cysteine (NAC), as a precursor of glutathione, helps to
replenish intracellular glutathione, a vital cellular antioxidant.
NAC has a low molecular weight and is well absorbed via oral
administration as compared to glutathione.
NAC may also protect against coagulation problems associated with
COVID-19, as it counteracts hypercoagulation and breaks down blood
clots.
Glutathione and Zinc
To improve your glutathione, you need zinc, and zinc in
combination with hydroxychloroquine (a zinc ionophore or zinc
transporter) has been shown effective in the treatment of
COVID-19.
Glutathione and Molecular Hydrogen
One of the best ways to increase glutathione, though, is molecular
hydrogen. Molecular hydrogen does so selectively and will not
increase glutathione unnecessarily if you don’t need it. You can
view Tyler LeBaron’s lecture on the details of how it does this in
“
How Molecular Hydrogen Can Help Your Immune System.”
Glutathione and Selenium
Selenium is also important, as some of the enzymes involved in
glutathione production are selenium-dependent.
Safety: As an FDA-approved drug, the safety profile of NAC has
been evaluated (Source) [
88]. Reported side effects of oral NAC include nausea, vomiting,
abdominal pain, diarrhea, indigestion, and epigastric discomfort (
Source). No safety concerns have been reported for products labeled as
dietary supplements that contain NAC.
NB: NAC supplements are not available on Amazon US. You
can buy NAC Supplements from Lazada Singapore.
8. Green Tea (EGCG)
Quercetin and EGCG act as zinc ionophores (
J. Agric. Food Chem. 2014), the same mechanism of action that hydroxychloroquine has via
helping zinc pass the cell wall where it might halt viral
replication.
Epigallocatechin-gallate (EGCG) 200mg (prevention) or 400 mg (early
treatment) 1 time a day
(J. Agric. Food Chem. 2014) is part of the Zelenko protocol for prevention and early treatment of COVID-19. EGCG acts
as a zinc ionophore and therefore needs to be combined with
zinc.
The strong oxidative stress-reducing and anti-inflammatory effects
of green tea catechins, including epigallocatechin gallate (EGCG),
have been well established. A solution of green tea catechins was
found to inactivate COVID-19 virus in the laboratory (
Ref).
Other laboratory and computer models suggest tea catechins may
inhibit viral infectivity and growth (
Ref). It has been proposed that EGCG, due to its immune-modulating
effect, could have a role in suppressing hyper-inflammation and
preventing lung fibrosis in patients with severe acute viral
respiratory illness (
Ref).
EGCG (Green Tea Extract), Quercetin, Zinc, Vitamin C and D -
Zelenko Prevention Protocol
Dr Zelenko's
prevention protocol recommends the following for COVID-19 prevention for Low
and Moderate Risk Patients:
2.1. Quercetin
(Amazon) 500mg 1 time a day until a safe and
efficacious vaccine becomes available. If Quercetin is
unavailable, then use
3. Vitamin D3 5000 iu 1 time a day (Amazon)
EGCG (Green Tea Extract), Quercetin, Zinc, Vitamin C and D -
Zelenko Treatment Protocol
Dr Zelenko's outpatient (over the counter options)
'treatment' protocol recommends the following for COVID-19 treatment
for Low Risk Patients:
1. Elemental Zinc 50mg 1 time a day for 7 days (PubMed)
2.1. Quercetin (Amazon)
500mg 2 times a day for 7 days (PubMed) OR
2.2. Epigallocatechin-gallate (EGCG) 400mg 1 time a day
for 7 days (J. Agric. Food Chem. 2014)
3. Vitamin D3 5000iu 1 time a day for 7 days (Amazon)
4. Vitamin C 1000mg 1 time a day for 7 days
9. Fish Oil (Omega-3 Fatty Acids) and Omega-6
Omega-3 fatty acids (omega-3s) are polyunsaturated fatty acids
that are present in
certain foods, such as flaxseed and fatty fish, as well as dietary
supplements, such as those containing fish oil. Several different
omega-3s exist, including alpha linolenic acid (ALA), but most
scientific research focuses on the long-chain omega-3s,
eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). The
main food sources of EPA and DHA are fatty fish and fish oil.
Omega-3s play important roles as components of the phospholipids
that form the structures of cell membranes (
Source). Omega-3s also form eicosanoids; these signaling molecules affect
the body’s cardiovascular, pulmonary, immune, and endocrine systems.
Omega-6 fatty acids, the other major class of polyunsaturated fatty
acids, also form eicosanoids, and these eicosanoids are generally
more potent mediators of inflammation, vasoconstriction, and
platelet aggregation than those made from omega-3s. Thus, higher
concentrations of omega-3s than of omega-6s tip the eicosanoid
balance toward less inflammatory activity.
Higher intakes
and blood levels of EPA and DHA are associated with lower levels of
inflammatory cytokines (
Source). Omega-3s might also affect immune function by up-regulating the
activity of macrophages, neutrophils, T cells, B cells, natural
killer cells, and other immune cells.
Omega-3 Fatty Acids and COVID-19
Omega-3 Fatty Acids are part of the
I-Recover treatment protocol for Long Haul or Post-COVID syndrome, launched on June
16, 2021 by the FLCCC (Front Line COVID-19 Critical Care
Alliance).
A
pilot study (Jan 2021) suggests that patients with the most omega-3s
in their system were 75% less likely to die from COVID-19. The
pilot study was conducted using blood drawn from 100 patients
treated for COVID-19 at the Cedars Sinai Medical Center in Los
Angeles. The postulated mechanism of action is the well known
anti inflammatory role of higher omega-3 levels, which may
helped quell the so-called 'cytokine storm' observed in some
severe and/or fatal COVID-19 cases.
This protection may have come from the effect EPA and DHA
have on the body. An opinion paper published in June 2020 in the
journal Frontiers in Physiology expounded on how "EPA and DHA
supplementation can alter many biological pathways which may have
a direct influence in the outcome of COVID-19."(
Front. Physiol., 19 June 2020) The writers listed the many nutrients that play a key role in
managing a cytokine storm and continued:
"Among these micronutrients, LC-PUFAs (long-chain
polyunsaturated fatty acids) such as EPA (eicosapentaenoic acid)
and DHA (docosahexaenoic acid) are noteworthy because of their
direct influence in the immunological response to viral
infections.
Among these complex immunomodulatory
effects, interleukin-6 (IL-6) and interleukin-1ß (IL-1β)—because
of the suspected central regulatory role in the "cytokine
storm"—should be highlighted."
The omega-3 fatty acids eicosapentaenoic acid (EPA) and
docosahexaenoic acid (DHA) modulate inflammatory processes in
the body through a variety of mechanisms (
Ref,
Ref). Severe acute viral respiratory infections can sometimes trigger
cytokine storm, in which excessive production of inflammatory
cytokines leads to uncontrolled systemic inflammation and
life-threatening tissue and organ damage. Another phenomenon, called
eicosanoid storm, has also been proposed to contribute to widespread
inflammation, tissue damage, and organ failure. Eicosanoid storm is
characterized by excessive production of pro-inflammatory and
procoagulant eicosanoids made from arachidonic acid, an omega-6
fatty acid synthesized in the body and obtained from dietary animal
fat (
Ref,
Ref). By competing with arachidonic acid for metabolic enzymes, EPA
and DHA decrease the production of pro-inflammatory and procoagulant
eicosanoids and increase production of specialized
inflammation-resolving compounds (
Ref,
Ref).
Accumulating evidence shows omega-3 fatty acids, administered
orally or intravenously, may help control inflammation and improve
outcomes in critically ill patients, including those with ARDS.489 A
meta-analysis of 12 randomized controlled trials with a total of
1,280 critically ill patients with ARDS found supplementation with
omega-3 fatty acids, in combination with gamma-linolenic acid (a
less-inflammatory omega-6 fatty acid) and antioxidants, improved
markers of lung function; however, only hourly administration,
rather than large bolus intravenous dosing, was associated with
reduced mortality. Although reductions in mechanical ventilation and
length of stay in intensive care were seen, these effects did not
reach statistical significance (
Ref).
An observational study in 100 patients hospitalized
with a severe acute viral respiratory illness found higher levels of
EPA plus DHA were associated with lower mortality, though the effect
was not statistically significant, possibly due to the small number
of participants (
Ref). During an outbreak of a severe viral respiratory infection,
another study found countries with the highest intake of omega-3
fatty acids from marine sources had lower mortality rates than other
regions of the world (
Ref). The same research group used computer modeling to show how
omega-3 fatty acids might bind to the highly infectious virus and
interfere with its ability to enter cells (
Ref).
Self-reported use of omega-3 supplements (dose not reported) more than
three times per week for at least 3 months among 372,720 U.K.
residents aged 16 to 90 years was associated with a 12% lower risk of
SARS-CoV-2 infection after adjustment for potential confounders (
Source). Findings were similar for 45,757 individuals in the United States
and for 27,373 participants in Sweden.
That are more than a dozen studies on-going that examine the
effect of EPA and/or DHA on the prevention of or lessening of
symptoms of COVID-19.
Evidence suggests the omega-3 fats EPA and DHA affect
biological pathways that may have direct influence in the
outcome of COVID-19.
EPA and DHA have a direct influence in the immunological
response to viral infections and can modulate immune response
and function.
Animal-based omega-3 fats, especially DHA, also help
prevent thrombosis (a blood clot within a blood vessel) by
decreasing platelet aggregation. Hypercoagulation is another
complication of severe COVID-19 infection that can have lethal
consequences.
Omega-3 also lowers your risk of lung dysfunction,
protects against lung damage and secondary bacterial
infections, and improves mitochondrial function.
Research shows that by lowering triglycerides, the risk
of developing a cytokine storm is diminished. Omega-3
supplementation is known to lower triglycerides, but krill oil
does so more effectively than fish oil.
The British Rhinological Society's Guidelines for the Management
of New Onset Loss of Sense of Smell During the COVID-19 Pandemic
advises that that fish oil supplementation (2,000 mg of omega-3
fatty acids/day) may be beneficial when used in addition to
standard treatment (olfactory training, oral steroids and steroid
rinses) (
Hopkins, Clin Otolaryngol 2020). This position is not based on a clinical trial of fish oil in
COVID-19 patients but on limited animal and human research
suggesting that omega-3 fatty acids may be beneficial for loss of
smell due to olfactory nerve damage.
An interesting development published in
Science, Nov 2020 revealed that linoleic acid (omega-6) binds with the 'spike
protein' of the COVID-19 virus and interferes with the entrance of
the virus into a human cell via the ACE-2
receptors. The study also revealed that in human cells,
Linoleic Acid supplementation synergizes with the COVID-19 drug
remdesivir in suppressing SARS-CoV-2 replication.
Safety: The FDA recommends not exceeding 3 g/day EPA and DHA
combined, including up to 2 g/day from dietary supplements (
Source). Some doses used in clinical trials exceed these amounts. The FNB
did not establish a
Tolerable Upper Intake Level
(UL; maximum daily intake unlikely to cause adverse health effects)
for omega-3s, although it noted that high doses of DHA and/or EPA (900
mg/day EPA plus 600 mg/day DHA or more for several weeks) might reduce
immune function by suppressing inflammatory responses (
Source).
Doses of 2–15 g/day EPA and/or DHA might also increase bleeding time
by reducing platelet aggregation (
Source). However, according to the European Food Safety Authority (EFSA),
long-term consumption of EPA and DHA supplements at combined doses of
up to about 5 g/day appears to be safe for adults. EFSA noted that
these doses have not been shown to cause bleeding problems or affect
immune function, glucose homeostasis, or lipid peroxidation.
Commonly reported side effects of omega-3 supplements—including
unpleasant taste, bad breath, heartburn, nausea, gastrointestinal
discomfort, diarrhea, headache, and odoriferous sweat—are usually
mild.
More information on omega-3s is available in the ODS
(Office of Dietary Supplements) health professional fact sheet on
omega-3s.
10. B Vitamins and COVID-19
Thiamine (vitamin B1), a water-soluble B-complex vitamin, is rapidly
depleted during times of metabolic stress, including severe illness.
Thiamine deficiency is common in hospitalized patients, especially
those with critical illness (
Ref). Thiamine is needed for cellular energy production and helps
regulate reduction-oxidation balance, immune function, nervous
system function, and vascular function (
Ref).
Thiamine, at 200 mg twice daily, reduced mortality in patients with
septic shock and thiamine deficiency, and laboratory research suggests
it may inhibit the hyper-inflammatory immune response that accompanies
cytokine storm (
Ref). It is a key therapeutic in the MATH+ protocol (methylprednisolone,
ascorbic acid [vitamin C], thiamine, and heparin, plus other
supportive nutrients and medications), a treatment strategy proposed
for managing advanced stages of severe acute viral respiratory illness
(
Ref). Although high-quality clinical evidence is lacking, two US
hospitals implementing the MATH+ protocol in patients with a severe
acute viral respiratory illness reported mortality rates that were
approximately one-quarter of those reported from other US hospitals
using standard care (
Ref).
In a study in Saudi Arabia (
Al Sulaiman et al. Crit Care 2021), 738 critically ill COVID-19 patients from two centers were
included in the study. The in-hospital death rate and 30-day death
rate were significantly lower in the group that received thiamine as
an adjunctive treatment (a therapy given in addition to standard
therapy). In addition, the thiamine group also were less likely to
have blood clot during ICU stay.
Another study of COVID-19 patients with severe symptoms found
26.3% among diabetics with COVID-19 were vitamin B1 deficient.
A study published in November 2020 from Singapore (
CW Tan, Nutrition 2020), found that those who were started on a daily oral dose of
vitamin D3 (1,000 IU), magnesium (150 mg) and vitamin B12 (500
mcg) within the first day of hospitalisation and continued up to
14 days were significantly less likely to require oxygen therapy
and further intensive care.
A
case series (published in September 2020) of 9 elderly COVID-19
patients treated with a combination of NMN, zinc, betaine and
sodium chloride resulted in rapid improvement.
The topic 'B vitamins' is a complicated subject and that's
probably why they are called 'B Complex'.
B vitamins may constitute a long list, but each one is important
for different reasons. B vitamins are especially effective in
boosting your immunity when you combine the foods containing them
so they can all work together for maximum effect. These include
vitamin B1 (thiamin), B2 (riboflavin), B3 (niacin), B5
(pantothenic acid) and B7 (biotin).
B12, also known as
cobalamin, is a powerful cold- and flu-fighting nutrient in your
system, as is vitamin B6, another important, germ-combating
vitamin that naturally benefits and strengthens your immune system
and even protects against the damaging effects of air
pollution.
Vitamin B9 and folic acid help repair
tissues and aid in cell metabolism and immune support. They’re
found in dark leafy greens, wild-caught, cold water fish like
herring, mackerel, sardines, anchovies and wild-caught Alaskan
salmon, and pastured, organic chicken.
Niacin or vitamin B3 is a precursor to nicotinamide adenine
dinucleotide (NAD+). There are
three main forms of niacin, which are dietary precursors to nicotinamide adenine
dinucleotide (NAD). These are nicotinamide riboside, nicotinic
acid and nicotinamide.
Nicotinamide adenine dinucleotide (NAD+) is an essential cofactor
in all living cells that is involved in fundamental biological
processes. NMN (Nicotinamide MonoNucleotide), is also another
precursor to NAD.
Adequate amounts of folate, vitamin B6 and vitamin B12 are also
needed for your body to make the amino acid cysteine. N-acetyl
cysteine (NAC) is a supplement form of cysteine. Consuming adequate
cysteine and NAC is important for a variety of health reasons —
including replenishing the most powerful antioxidant in your body,
glutathione.
11. Molecular Hydrogen

There have been a plethora of studies on hydrogen’s effects on
inflammation, in particular in regulating/controlling inflammatory
cytokines. For example:
-
A group of scientists in China suggested that hydrogen-rich solution
therapy may be a safe, reliable, and effective treatment for
Multiple Organ Dysfunction Syndrome (MODS) induced by influenza and
other viral infectious diseases (SOJ Microbiol Infect Dis. 2017).
-
In a 2017 lab study published in the World Journal of
Gastroenterology, “HRW (hydrogen rich water) treatment significantly reduced
EtOH-induced increases in serum alanine amino transferase, aspartate
aminotransferase, triglycerol and total cholesterol levels, hepatic
lipid accumulation and inflammatory cytokines, including tumor
necrosis factor-alpha (TNF-α) and interleukin (IL)-6.”
-
Another study in 2013 stated “The serum levels of cytokines such as IL-10, TNF-α,
IL-12p70, and GM-CSF of mice administered with HW (hydrogen water)
was significantly reduced as compared to PW (placebo water) group.”
There are at least 30 other high-impact scientific studies that mention
hydrogen’s observed balancing and lowering effect on inflammatory
cytokines.
Beyond the existing scientific studies that show a
reason for excitement, hydrogen gas is also now being recommended in
China as a therapy for individuals suffering from COVID-19, and there
are very positive recorded anecdotal reports from patients.
The first preliminary report on COVID-19 patients (n=90) from China
has been published demonstrating that Hydrogen/Oxygen mixed gas
inhalation has superior effects compared to Oxygen alone (
Journal of Thoracic Disease. 2020).
The science behind the virus and potential treatment is, of course, far
more complex than this, and we do not intend to simplify the situation
whatsoever. Nonetheless, the potential here is interesting — especially
when you factor in the safety factor of molecular hydrogen. We will have
to see what happens as the science develops and the clinical trials are
conducted, and we will update this article with more information as it
becomes available.
12. Selenium
Selenium plays a role in immune cell function and activation through
its incorporation into enzymes and other proteins. It also reduces
infectivity, replication, and virulence of several respiratory viruses
(
Ref). Sodium selenite, a form often used in supplements, has been
found to block an infectious respiratory virus from entering cells by
interacting with its spike protein in the laboratory (
Ref).
Selenium works closely with vitamin E and cysteine to regulate
oxidation and reduction balance and neutralize free radicals, and can
help reduce inflammatory signaling by controlling oxidative stress (
Ref). Poor selenium status may also increase the likelihood of induction
of excess inflammation due to cytokine storm (
Ref).
The soil concentration of selenium varies geographically around
the world, affecting selenium status and resulting in endemic
insufficiency and deficiency (
Ref). A study comparing COVID-19 survival to regional selenium status
during a major outbreak in China found survival was more likely in
high-selenium regions (
Ref). A study done during an outbreak in Germany found higher selenium
and selenium-containing protein levels in COVID-19 infection survivors
versus non-survivors (
Ref).
Blood selenium levels have been noted to diminish in
patients with critical illness, and lower levels are correlated with
more severe illness and lower chance of survival (
Ref). A meta-analysis of 19 randomized controlled trials found
intravenous selenium supplementation in critically ill patients
reduced total mortality (but not 28-day mortality) and shortened the
length of hospital (but not intensive care unit) stay (
Ref).
In a randomized controlled trial in 40 patients with ARDS, those who
received sodium selenite intravenously for 10 days had increased
glutathione levels, decreased inflammatory cytokine levels, and
improved lung function compared with those who received saline
(placebo). However, there were no differences in survival or intensive
care unit stay (
Ref).
13. Probiotics
Probiotics are live microorganisms that confer a health benefit on the host
when administered in adequate amounts (
Source). They include certain bacteria (e.g., Lactobacillus acidophilus,
Lactobacillus rhamnosus, and Bifidobacterium longum) and yeasts (e.g.,
Saccharomyces boulardii). Probiotics are naturally present in some fermented
foods, added to some food products, and available as dietary supplements.
Probiotics
act mainly in the gastrointestinal tract (
Source). They might improve immune function in several ways, including
enhancing gut barrier function, increasing immunoglobulin production,
inhibiting viral replication, and enhancing the phagocytic activity of white
blood cells. However, the mechanisms of their potential effects on immune
function are unclear. In addition, research findings for one probiotic strain
cannot be extrapolated to others.
Through the mesenteric lymphatic system, intact bacteria and their
metabolites enter the circulation and influence the lung immune response
(gut/lung axis). Through this way intestinal metabolites, mainly produced by
bacterial fermentation of dietary fiber, such as short-chain fatty acids
(SCFAs), significantly influence local gut immunity but also distant organs.
SCFAs derived from gut are able to suppress lung inflammation (
Ref). Dendritic cells (DCs), the antigen-presenting cells of the immune
system, stimulate T-cells subpopulations in mesenteric lymph nodes and gut
lymphatic tissue to produce regulatory cytokines. After airways
immune-stimulation, these T-cells move from the gut to the respiratory
system, providing protection and stimulating an anti-inflammatory response.
In fact, gut microbiota rebalancing has been shown to reduce
ventilator-associated enteritis and pneumonia (
Ref).
Altered bacterial balance (dysbiosis) causes the translocation of cytokines,
endotoxins and microbial metabolites in the general circulation to other
organs, such as the lung. Conversely, respiratory inflammation (due to many
causes, e.g., respiratory viral infections due to COVID-19 virus), causes
local dysbiosis and, in turn, the translocation of microbial metabolites and
toxins to other organs, such as the gut (below).
Physiological changes in the human microbiota with age leads to a
“physiological dysbiosis”, with less diversification in microbial
composition, aggravated in case of comorbidity (hypertension, diabetes,
chronic inflammatory bowel diseases, etc.) (
Ref). Therefore, to establish the condition of eubiosis (healthy condition),
“good” bacteria are required. The concept of probiotics as a food with
positive effects was firstly used by Parker RB in 1974 and then recognized
by the Food and Agriculture Organization (FAO), and more recently by the
Word Health Organization (WHO) (
Ref).
Multiple randomized controlled trials and several meta-analyses have shown
probiotics reduce the risk of acute respiratory tract infections (eg, colds
and flu) (
Ref).
Two meta-analyses of twelve and thirteen randomized controlled trials (
Diabetes Metab Syndr. 2021), demonstrated clinical benefits of Lactobacillus and Bifidobacterium
administration in mechanically ventilated patients in ICU, showing a lower
incidence of upper respiratory tract infections and ventilator-associated
pneumonia.
Self-reported use of probiotic supplements more than three times per week for
at least 3 months among 372,720 U.K. residents aged 16 to 90 years was
associated with a 14% lower risk of SARS-CoV-2 infection after adjustment for
potential confounders (
Source). Findings were similar for 45,757 individuals in the United States and for
27,373 participants in Sweden.
Another clinical study in Italy showed a better prognosis in 28 of 70
symptomatic patients taking probiotics (L. acidophilus DSM 32241, L.
helveticus DSM 32242, L. paracasei DSM 32243, L. plantarum DSM 32244, L.
brevis DSM 27961, B. lactis DSM 32246, B. lactis DSM 32247, 2400 billion
bacteria per day), reducing the risk of admission in ICU. All these actions
would be useful in reducing SARS-CoV-2 dissemination in the respiratory tract
and gut, reinforcing both anti-inflammatory responses and immune
defenses
(Ref).
Recently, several peer-reviewed reports of clinical experiences, preclinical
studies, small, open clinical trials, case series, and clinical hypotheses
have suggested that certain immune-modulating probiotic strains, such as L.
rhamnosus CRL-1505 (
Ref), Streptococcus salivarius K12 (
Ref), L. plantarum LP01 (
Ref), and B. lactis BS01 (
Ref) may confer protection against respiratory viral infections and/or
subsequent inflammatory sequela.
The first quadrupled blinded randomised controlled trial (
MedRxiv May 2021) on a novel probiotic formulation demonstrated that complete remission on
day 30 was boosted from 28% to 53%.
Numerous
clinical trials to investigate the usefulness of probiotics in treating severe acute
viral respiratory infections have been registered since early 2020, and many
are currently underway.
Safety: Probiotics, such as strains of Lactobacillus, Bifidobacterium,
and Propionibacterium, have a long history of use in food and are often
present in the normal gastrointestinal microbiota, indicating that probiotic
supplements are safe for most people (
Source). Side effects, which are usually minor, include gastrointestinal symptoms,
such as gas. However, potential safety concerns can include systemic
infections, especially in individuals who are immunocompromised. For example,
in a few cases (mainly in individuals who were severely ill or
immunocompromised), the use of probiotics was linked to bacteremia, fungemia
(fungi in the blood), or infections that resulted in severe illness.
More
information on probiotics is available in the ODS health professional fact
sheet on
probiotics.
14. Lactoferrin
Lactoferrin is an iron-binding protein made by cells such as those in
secretory glands and activated neutrophils (a type of immune cell). It is
found in most bodily fluids, including tears and breast milk, and lactoferrin
derived from bovine whey is frequently used in supplements (
Ref). Lactoferrin is an immune modulator, capable of enhancing antimicrobial
immune activity while reducing inflammation, and has exhibited a broad
spectrum of activity against bacteria, fungi, protozoa, and viruses (
Ref). Laboratory research also suggested lactoferrin may inhibit entry of a
highly infectious respiratory virus into cells by blocking its interactions
with cell membrane components (
Ref).
Lactoferrin may slow pathogen multiplication through its iron
binding capacity. While iron is required for DNA replication and energy
production, the presence of excess iron increases free radical generation,
stimulates inflammatory processes, and exacerbates viral infection by
promoting increased viral replication (
Ref). Furthermore, patients with a severe acute viral respiratory infection have
been found to have elevated levels of ferritin, and these levels correlated
with increased risk of death (
Ref). In its iron-free state (apolactoferrin), lactoferrin can sequester
pro-oxidant free iron, lowering oxidative stress and suppressing the growth of
pathogens, and possibly mitigating the serious complications of infection (
Ref).
In a pilot trial, 75 patients who tested positive for an acute
viral respiratory tract infection were treated at home with a liposomal
preparation of a combination of 32 mg bovine lactoferrin with 12 mg vitamin C,
with or without 10 mg liposomal zinc, four to six times daily for 10 days. In
addition, lactoferrin nasal drops, mouth spray, and aerosol were used as
needed by participants with headaches, loss of sense of smell and taste, nasal
congestion, dry cough, or difficulty breathing. After 48 hours, all symptoms
had diminished except loss of smell and taste, and by day five, all infected
participants recovered from their illness with only loss of smell and taste
remaining as residual symptoms (
Ref).
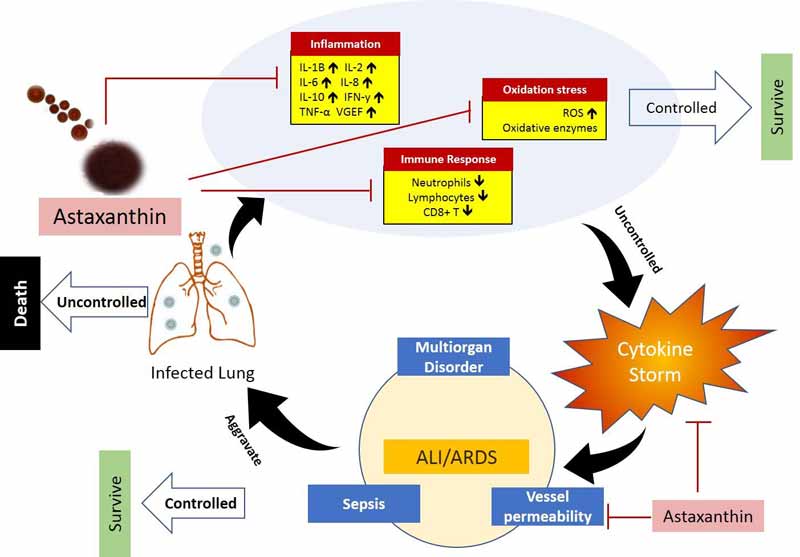
15. Astaxanthin
The paper (
SSRN) “COVID-19: Potential of Microalgae Derived Natural Astaxanthin
as Adjunctive Supplement in Alleviating Cytokine Storm,” published April
21, 2020, on the research library website SSRN, addresses the use of
astaxanthin, a potent antioxidant supplement derived from microalgae.
The full paper is downloadable from the link.
As explained in
this paper, astaxanthin has a very unique molecular structure that
allows it to penetrate the bilayer membrane of cells. The ability to
quench reactive oxygen species (ROS) and free radicals in both the inner
and outer layers of the cellular membrane allows it to provide superior
protection against oxidative stress, compared to other antioxidants.
Vitamin
E and beta-carotene, for example, only work in the inner side of the
membrane, and vitamin C only works on the outer side.
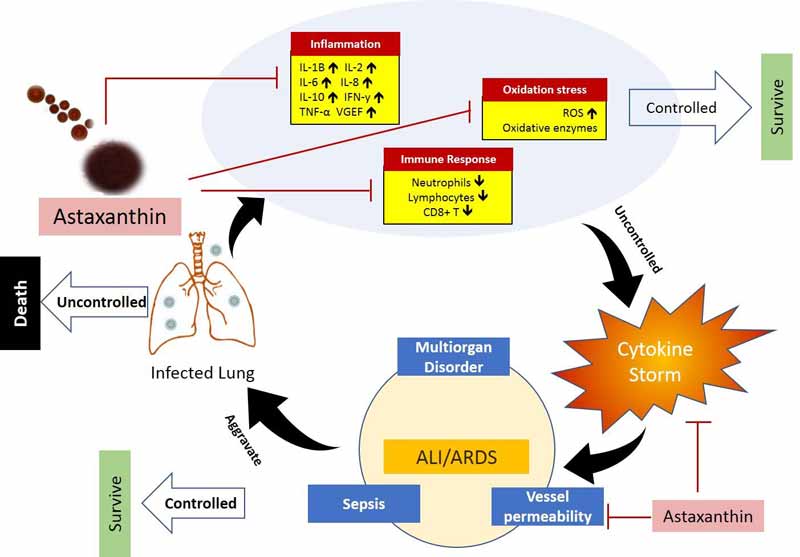
In short, astaxanthin ticks many important boxes when it
comes to ameliorating COVID-19, including immune response regulation and
the enhancement of both cell-mediated and humoral immune responses, as
well as the simultaneous protection against oxidative damage and
inflammation.
Conclusion
Macronutrients and micronutrients are essential to a human body, there are
no ifs and buts about it. Optimizing your immune system is critical to
improve your health whether there is a pandemic or not.
Optimizing
your immune system with diet and lifestyle changes are critical to improving
your health and to decrease your risk with COVID-19. However, therapeutics,
vaccines and other physical strategies such as social distancing and mask
wearing are also needed in order to protect yourself and your loved ones. It
doesn't have to be an 'either or' situation. Combination strategies are
normally more effective.
Nutritional supplements are meant to tip the scales in favour of you in terms
of your immune system and to improve your probability of a smooth recovery, if
at all you do get COVID-19. You still need to follow the advice given by CDC,
WHO and your local authority in terms of local guidelines.



.png)
.png)







Comments
Post a Comment