Why Aren’t Interventional Pain Management Physicians Offering More Regenerative Solutions?
Chris Centeno MD - These past few years I’ve seen that while regenerative medicine is gaining wider acceptance, there’s been an explosion in treatments being offered that aren’t nearly as elegant. What fits into that category and why does it make me uncomfortable? Let’s dig in.
More Options are Better than Fewer
The great thing about helping patients in pain these days is that there are many options. In addition, while some of the things discussed below aren’t as good as regenerative options, sometimes patients do need these procedures to feel better. Hence, my focus here is on helping physicians realize an aspirational goal.
The Main Types of Interventional Pain Management
IPM or Interventional Pain Management is a field where the doctor uses precise image-guided procedures that don’t involve open surgery that can help patients in chronic pain. These are percutaneous procedures, meaning they can generally be performed without a scalpel and “through the skin”.
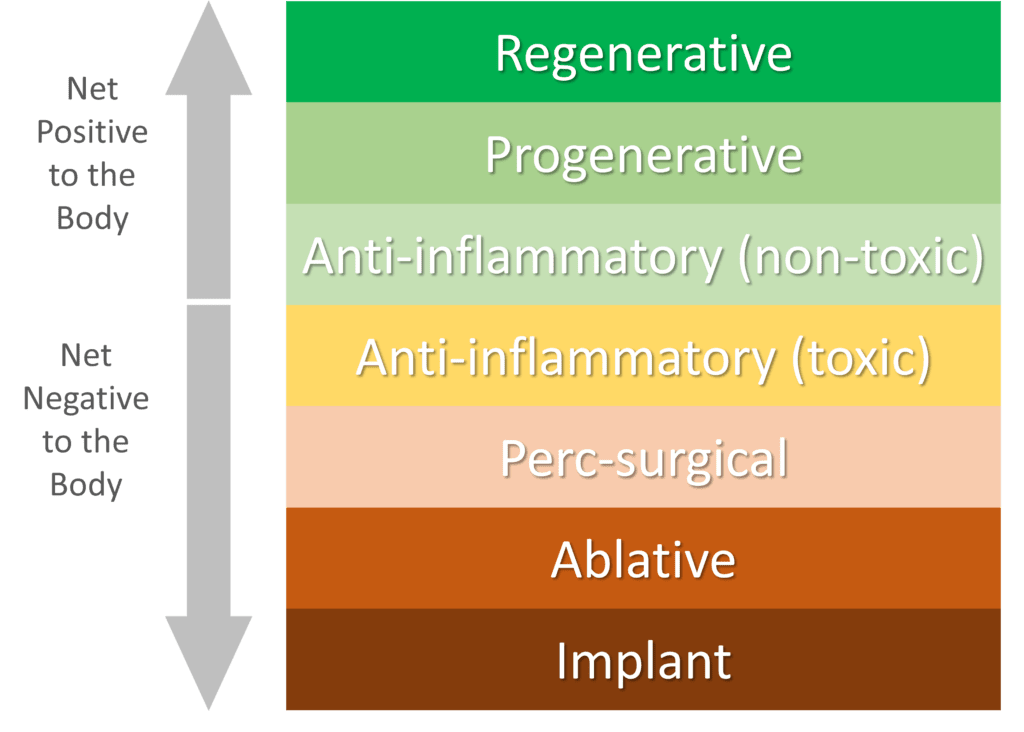
While all percutaneous procedures are an improvement over open surgery, it’s critical that we begin to look at how different types of procedures impact the body. Meaning are some better than others if one can accomplish the same goal as the other? My answer to that question is a resounding “Yes”. So let’s break these IPM approaches into categories on how they impact the body from best to worst:
- Regenerative—The procedure causes new or stronger tissue to regrow and/or repairs damaged tissue.
- Progenerative—These procedures have a positive impact on the microenvironment. For example, they make the area healthier and more similar to normal tissue but don’t regenerate damaged tissue.
- Anti-inflammatory (non-toxic)—This is a chemical drug that can reduce inflammation, but doesn’t damage local tissues.
- Anti-inflammatory (toxic)—A chemical drug that reduces inflammation, but is known to damage local tissues.
- Perc-Surgical—A procedure that cuts or removes tissue, but does so through the skin (percutaneous).
- Ablative—This procedure destroys painful tissue or nerves that carry pain signals.
- Implant—A procedure to place a foreign object in the body to help pain.
Let’s dive deeper into each one of these categories:
Regenerative
The ultimate goal of medicine is to be able to regenerate damaged tissue. That’s the pinnacle of what every doctor should strive for and there is nothing better. For example, your tendon is damaged, so let’s grow you a new one. Or your nerve is scarred and in poor health, so let’s perform a procedure to make it like new. No anti-inflammatory, surgery, ablative procedure, or implant could hope to come close to that kind of therapeutic efficacy and elegance. When it comes to positive versus negative impacts on the body, there is simply nothing better.
So what’s in this category now? Here’s a brief list of what I have observed in clinical practice using orthobiologics like PRP, platelet lysate, bone marrow concentrate (BMC), and culture-expanded mesenchymal stem cells:
- Small cartilage lesions in joints can sometimes be healed with BMC or culture-expanded MSCs
- Tendons, ligaments, and tears in spinal discs can be repaired using high-dose PRP, BMC, or culture-expanded MSCs
- Degenerative spinal discs can be made to hold onto water on a case by case basis (meaning the effect is not reliable) with PRP, BMC, or culture-expanded MSCs
- Nerve injury can be helped by PRP, platelet lysate, and culture-expanded mesenchymal stem cells
Progenerative
I coined this term this morning to mean an orthobiologic that can help damaged tissue act more like normal, but that falls short of repairing it fully. So while not as good as growing new tissue to replace damaged tissue, it’s almost as good because it has no serious toxic side effects and it markedly increases function. In addition, some of the things in this category may slow the degenerative cascade, which doctors call “disease-modifying”. Again, this is a net positive for the body.
What’s in this category now?
- Arthritis can be helped and perhaps slowed by PRP, A2M, BMC, and culture-expanded MSCs. The effect seems to be the biggest and longest for BMC and the MSCs.
- Degenerative Disc Disease-PRP and PL can reduce degenerative instability and improve function long-term.
- Radiculopathy can be improved with PRP and PL.
- Severe tendon degeneration can be improved and perhaps slowed by using PRP and BMC.
Anti-inflammatory (non-toxic)
As recent research has shown, blocking inflammation is likely not an elegant long-term solution to any pain problem as it blocks the body’s ability to resolve the problem. However, when an anti-inflammatory has to be used to provide quick and easy relief, in our clinical experience, reducing the dose of a corticosteroid into the nanogram range seems to have few side effects and still provides a potent reduction in swelling. I suspect that we’ll see lots of cytokine and growth factor based drugs in the next 10-20 years that can manage inflammation in this elegant way.
Anti-inflammatory (toxic)
This is the classic IPM “steroid injection” which is a high dose (milligram or a million times more than the nanogram physiologic dose the body uses). While a potent anti-inflammatory that can provide short-term relief, it’s clearly toxic to local tissues. Meaning, that it’s a net negative to the body.
Perc-Surgical
The goal of many surgeries is to remove or cut tissue. The problem is that in the body, there are no spare parts. Meaning while this type of procedure may need to be done in select patients, it’s always damage to accomplish a goal. While percutaneous surgical procedures like removing a disc bulge through a scope are better than open procedures, they still suffer from the same problem as open surgeries. For example, we know that while removing part of the outer disc that’s bulging may help a spinal nerve that’s getting irritated, the disc is now more likely to herniate in the future because there is less tissue holding the nucleus pulposus (center of the disc) back. Or while cutting the transverse carpal ligament in the wrist can reduce carpal tunnel symptoms, it also destabilizes the wrist.
Ablative
In medicine, to “ablate” is a fancy term that means to destroy. In IPM, there are many procedures like RFA (Radiofrequency Ablation) that ablate the nerves carrying pain signals. The problem? Those nerves have other functions and eventually grow back, often making the pain worse than it was before. For example, you can ablate the nerve that carries pain signals from the facet joints in the low back, which can help back pain. However, that nerve also supplies the critical multifidus stabilizing muscles that protect the low back from damage. So ablating these nerves is a net negative for the body. You can do the same for the cervical facets, but after a decade of experience doing that to patients, their pain invariably comes back worse once the effects of the ablation wear off.
Implants
There is nothing ever devised that you can place in the body that’s natural. Meaning if you place a piece of metal in the body, even if that’s placed in a less invasive way, that’s still a foreign object. We also know that these metals leech into the patient’s bloodstream and impact some patients more than others, with metal allergies now being a problem. Finally, that piece of metal or ceramic or plastic will eventually wear out, as it has no ability to repair and maintain itself.
This is perhaps the biggest growth area in IPM I have seen that concerns me. For example, we know from many studies that fusion is always a bad idea in that it leads to adjacent segment disease and abnormal motion. However, my colleagues are now placing SI joint fusion screws with wild abandon. Another problem is “interspinous spacers” which are used to treat spinal stenosis. These destroy the supra and interspinous ligaments with spine surgeons reporting that these devices are failing at an alarming rate, requiring their removal. Finally, placing implantable nerve stimulators to block pain signals is now a big thing. However, in the long run, my experience to date shows that these systems don’t last and often need to be removed or revised. In the end, none of these implantable solutions are as elegant as regenerating or helping maintain natural tissues.
Why Not Just Always Focus on the Top Three Positive Options?
Common sense would dictate that 9 in 10 times, the best way to help pain would be Regenerative, Progenerative, or reducing inflammation more naturally. However, that type of care is only offered to a small percentage of patients each year. Why? The most often cited reason is insurance coverage. Meaning the other options are easier to get an insurance company to cover. However, that argument no longer really holds water. Why? Co-pays, co-insurance, deductibles, and other out-of-pocket expenses for private insurance frequently cost as much as the out-of-pocket expenses for the regenerative options. So why don’t more doctors insist on those easier on the body regenerative approaches? The real reason, if I’m being frank, is that it’s easier to bill the patient’s insurance and let them worry about out-of-pocket costs than it is to talk to the patient about better options that will require an out-of-pocket expense.
Read More: https://regenexx.com/blog/ipm-regenerative/
.png)

.png)






Comments
Post a Comment