Is Blocking Acute Inflammation Causing Chronic Pain?
We’ve known for a long time that injecting high-dose steroids into patients to treat pain is a dumb idea. However, that was based on studies showing harm to the local tissues. What if it’s also creating millions of new chronic pain patients? Let’s dig in.
Natural and Mega Dose Steroids
The issue with medicine’s steroid addiction when treating pain is a dose problem. When Cortisone first hit the market in 1948, the best technology that the period could muster was to provide it in a milligram dose. That might not sound like much, but to the body, which is used to seeing nanogram doses of this same type of substance, it’s like using a sledgehammer to put in a tack. It works, but the results aren’t pretty. Let’s explore that dose difference.
A milligram is a thousandth of a gram. A nanogram is a billionth of a gram. To understand the massive difference between the two, let’s use everyday objects. If the height of a soda can represents a nanogram, then the height of a satellite orbiting the earth represents a milligram.
Now let’s see how cells react to these two different doses. If I take 50 nanograms of a steroid drug and place that into a culture with mesenchymal stem cells, they react in predictable ways. For example, if I combine that natural dose of steroid with a few other drugs, the cells will stay healthy and turn into cartilage cells. However, if I add 1 milligram of the same steroid drug into that culture (1,000,000 times more), every cell will be dead or dying within hours. That experience almost two decades ago helped me understand just how toxic mega doses of steroids were to the body’s cells.
The Effects of Mega Dose Steroids on Tissues
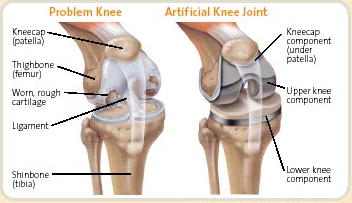
We’ve known for a VERY long time that mega-dose steroids harm tissues (1-7). That includes the mesenchymal stem cells described above as well as the cartilage cells in knees. In addition, they do so much damage to the local immune response that they markedly increase the risk for infection if that joint is later operated on.
As a result, we stopped using all mega-dose steroids in our practice almost two decades ago. Instead, we get steroids specially compounded into natural nanogram doses. They still work fine, but without all of the nasty side effects.
NSAIDs
Another common practice in modern orthopedics is the idea that acute pain should be treated with oral anti-inflammatory drugs. Nonsteroidal Antiinflammatory Drugs (NSAIDs) are common and include a bevy of trade names like Motrin, Advil, Alleve, Naprosyn, Celebrex, Voltaren, and Indocin. They work by blocking inflammation at the cyclo-oxygenase (COX) pathway.
We’ve known for some time that NSAIDs can impair bone healing (8). Data suggest that NSAIDs reduce new collagen manufacture, which is required to heal the wear and tear on tendons. However, good clinical research on the effects of these drugs on the healing of orthopedic injuries is hard to find. Why? See my comments below on the anti-inflammatory industrial complex.
Do Mega-Dose Steroids and NSAIDs Cause Chronic Pain?
Researchers from McGill University recently published in the medical journal Science Translational Medicine looking at how chronic pain takes hold in both mice and humans (9). The team determined that what separates patients whose pain resolves quickly from those who develop chronic pain is how their bodies use a key inflammatory cell called neutrophils. Experimentally blocking neutrophils in mice with an acute injury prolonged their pain by up to ten times the normal duration. Treating those same animals with mega-dose steroids or NSAIDs produced the same result. These findings were also supported by an analysis of 500,000 people in the UK which showed that those taking NSAIDs for pain were more likely to develop chronic pain 2-10 years later. This effect wasn’t seen in patients taking Tylenol.
The Anti-inflammatory Industrial Complex
If we’ve known for some time that mega-dose steroids and NSAIDs are a problem, why then are these the most commonly prescribed drugs for acute pain in the world? The first is simple, insurance reimbursement. These drugs are still paid for by carriers who have failed to get the memo, even though study after study continues to show that insurers are costing employers more money by reimbursing their use. The second is institutional momentum. Doctors are taught in medical school not to rock the proverbial boat; hence mega-dose steroids and NSAIDs continue to make it into every large organization’s treatment guideline despite new evidence of harm. Finally, there are the companies that make these drugs or reformulate them to gain new FDA approvals and eek more money out of a concept first developed in the 1940s. Go to any orthopedic conference and you’ll see what I mean. You can bet that Pfizer has a massive Celebrex booth costing 50-100K.
The upshot? Note to colleagues; please STOP prescribing these drugs to patients with pain from injuries! They are clearly toxic, and at some point, their prescription will quickly morph from standard of care to medical malpractice.
_____________________________________________________
References:
(1) Wyles CC, Houdek MT, Wyles SP, Wagner ER, Behfar A, Sierra RJ. Differential cytotoxicity of corticosteroids on human mesenchymal stem cells. Clin Orthop Relat Res. 2015 Mar;473(3):1155-64. doi: 10.1007/s11999-014-3925-y. Epub 2014 Sep 4. PMID: 25187334; PMCID: PMC4317436.
(2) Dragoo JL, Danial CM, Braun HJ, Pouliot MA, Kim HJ. The chondrotoxicity of single-dose corticosteroids. Knee Surg Sports Traumatol Arthrosc. 2012 Sep;20(9):1809-14. doi: 10.1007/s00167-011-1820-6. Epub 2011 Dec 21. PMID: 22186921.
(3) McAlindon TE, LaValley MP, Harvey WF, et al. Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial. JAMA.2017;317(19):1967–1975. doi: 10.1001/jama.2017.5283
(4) Wijn SRW, Rovers MM, van Tienen TG, Hannink G. Intra-articular corticosteroid injections increase the risk of requiring knee arthroplasty. Bone Joint J. 2020 May;102-B(5):586-592. doi: 10.1302/0301-620X.
(5) Richardson SS, Schairer WW, Sculco TP, Sculco PK. Comparison of Infection Risk with Corticosteroid or Hyaluronic Acid Injection Prior to Total Knee Arthroplasty. J Bone Joint Surg Am. 2019 Jan 16;101(2):112-118. doi: 10.2106/JBJS.18.00454.
(6) Ravi B, Escott BG, Wasserstein D, Croxford R, Hollands S, Paterson JM, Kreder HJ, Hawker GA. Intraarticular hip injection and early revision surgery following total hip arthroplasty: a retrospective cohort study. Arthritis Rheumatol. 2015 Jan;67(1):162-8. doi: 10.1002/art.38886.
(7) Forsythe B, Forlenza EM, Agarwalla A, Cohn MR, Lavoie-Gagne O, Lu Y, Mascarenhas R. Corticosteroid Injections One Month Before Arthroscopic Meniscectomy Increase the Risk of Surgical Site Infection. Arthroscopy. 2021 Mar 31:S0749-8063(21)00289-9. doi: 10.1016/j.arthro.2021.02.047. Epub ahead of print. PMID: 33812029.
(8) Lisowska B, Kosson D, Domaracka K. Positives and negatives of nonsteroidal anti-inflammatory drugs in bone healing: the effects of these drugs on bone repair. Drug Des Devel Ther. 2018;12:1809-1814. Published 2018 Jun 21. doi:10.2147/DDDT.S164565
(9) Parisien M, Lima LV, Dagostino C, El-Hachem N, Drury GL, Grant AV, Huising J, Verma V, Meloto CB, Silva JR, Dutra GGS, Markova T, Dang H, Tessier PA, Slade GD, Nackley AG, Ghasemlou N, Mogil JS, Allegri M, Diatchenko L. Acute inflammatory response via neutrophil activation protects against the development of chronic pain. Sci Transl Med. 2022 May 11;14(644):eabj9954. doi: 10.1126/scitranslmed.abj9954. Epub 2022 May 11. PMID: 35544595.
Source: https://regenexx.com/blog/is-blocking-acute-inflammation-is-causing-chronic-pain/
About the Author: Chris Centeno, MD is a specialist in regenerative medicine and the new field of Interventional Orthopedics. Centeno pioneered orthopedic stem cell procedures in 2005 and is responsible for a large amount of the published research on stem cell use for orthopedic applications.
.png)

.png)



.png)


Comments
Post a Comment