The Mystery Behind India’s Success in Flattening the Curve
On January 30, 2021, India completed one year since the first Covid-19 case was detected in India from Kerala. At the start of the pandemic, India as a country was very vulnerable for a major coronavirus outbreak. Not only is India the world’s second most populous country, it has some of the most congested cities with an average population density of around 470 people per square km. Add to it, the lack of a robust healthcare infrastructure which was already overburdened. From the beginning, many experts from the western countries have been predicting doom for India. The US-based Center for Disease Dynamics and Economic Policy (CDDEP), had in its report dated April 20 said India’s total SARS-CoV-2 infections up to September 2020 could be as high as 1.11 billion, even with “hard lockdown, continued social distancing and isolation of cases”. There were worries expressed by them about the entire Indian healthcare infrastructure crumbling under the burden of the outbreak, while central government of India worked tirelessly and meticulously steering the country on the right path.
ICMR (Indian Council for Medical Research) was the first national research agency in the world who not just understood the importance of the primary care in taming this pandemic, but also recommended treatment with specific medicines and identified regimens for each grade of Covid-19 patients. This was a masterstroke that none of the foreign agencies including CDC (USA), NHS (UK) & others have been able to deliver. All medical authorities continued to say that there is no early treatment available to treat mild cases at home but kept ramping up hospital beds & ventilators which continued to fall short of requirements. While the central & state govts. in India ramped up healthcare infrastructure like never before, they depended tremendously on the primary care clinics and doctors to face the brunt and treat aggressively with recommended regimens. We could thus beat all projections of hundreds of millions with cumulatively little more than 11 million cases. As we look back, it would be interesting to trace the hidden footsteps of success to solve the mystery of flattening the curve since the western experts have already started making their own conclusions in mainstream media.
India’s journey from “Gloom to Resume”
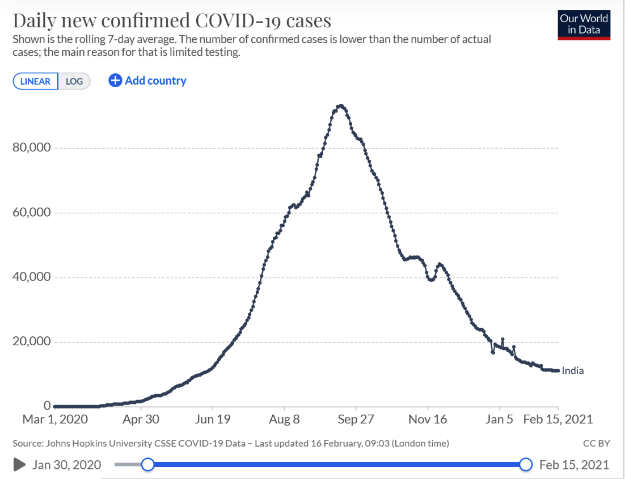
The cases in India climbed steadily from April to September 2020, reaching a peak of nearly 100K daily cases on September 16. Hospitals were filled to capacity and patients had to be turned away due to lack of beds; admissions were not guaranteed even for severe cases. Then, things took an unexpected turn. India’s daily cases plummeted from mid-September through January, with average weekly cases dropping off by roughly a third each month. India is now reporting around 10,000 daily cases on an average. Hospital beds created for this purpose are now in excess and several Covid-19 facilities in the big cities have been closed. Health minister Dr Harsh Vardhan, has rightfully claimed that India has “successfully contained the pandemic” and “flattened its Covid-19 graph”.
Analyzing theories behind the mystery:
Let us analyze all potential reasons behind this success and try validating each based on available data. Following are the theories that are being touted to explain this dramatic drop in cases. The most prominent are:
Prevalent Infections like TB, Malaria, etc. – This theory proposes that the immunity to other infectious diseases like TB & malaria could have helped Indians fight Covid-19 better than their western counterparts where these diseases are rare. While this idea is very attractive due to the new focus on T cell immunity for Covid-19 which was always known for TB like infections, there is no evidence to prove the same. There are 13 Phase 3 and 7 Phase 4 clinical trials that are currently ongoing to investigate whether BCG vaccination can induce immunity against Covid-19. However, the jury is still out in terms of trial results. Since BCG vaccine is used in many parts of the world to prevent TB, its use to prevent Covid-19 has not been recommended by any agency in the world due to lack of evidence. Similarly, the connection of malaria and Covid-19 came up due to 2 reasons. Firstly, due to relatively lesser case density of Covid-19 in malaria affected countries like sub-Saharan Africa. Secondly, due to the use of Hydroxychloroquine (HCQ) for both conditions. However, other countries like S. Africa were impacted much worse with a new resistant mutant developed there, lessening the importance of this theory as well.
Demographics – India is a very young country in demographics. Only 6% of Indians are older than 65 and more than half the population is under 25. Those who are young are more likely to socially interact and spread the disease but less likely to die of Covid-19. Whereas elderly population is less likely to move around but more likely to get hospitalized and die if infected. This might have played a major role in faster spread in India and lesser mortality but doesn’t explain the sudden drop in cases post September.
Alpha1-antitrypsin Deficiency – Recently there were several reports that claimed AAT (alpha1-antitrypsin) deficiency in European and North-American populations as a possible reason why the mutated SARS-CoV2 was able to spread faster in those countries as compared to India. The mechanism proposed in the study was that AAT has an inhibitory action on elastase, an enzyme which specifically helps in the entry of D614G mutated virus into the cells. Hence, the hypothesis said that if AAT levels are low, elastase will not get suppressed and will help the mutated virus gain entry into the cells. Firstly, this theory has not been demonstrated through experiments in the lab. Secondly, the news report indirectly suggests that Indian population does not have such a deficiency, hence coronavirus did not spread as quickly in our country. However, upon closer look at the article, we saw that the analysis only included East Asian countries like Indonesia, Philippines, South Korea etc. The article does not include AAT deficiency data of Indian population. Moreover, per the study conducted in October 2020, D614G mutation was already prevalent in India, being responsible for almost 70% of the cases. If AAT was able to specifically prevent D614G mutated virus from spreading in Indian population, we would not have seen such a high prevalence of the same mutation here. Therefore, we can discard this theory to explain India’s success over Covid-19.
Strict Lockdown & Mask Mandates – Several large cities and states in India began requiring masks in public places since April, 2 months before the World Health Organization recommended masks for the general public. Metro cities like Mumbai and Delhi also imposed fines for not wearing masks in public places. For the most part, Indians have been supportive of mask requirements in contrast to the US, which is vertically split on whether masks are effective. While initially experts had denied that this infection can be airborne when they were recommending masks, subsequently there was new understanding that this infection may be transmitted through air. If it is an airborne virus, masks have a diminished role for protection. In any case, it can’t be solely responsible for the drop in cases nor unique to India’s approach as other countries following mask mandate haven’t seen such flattening of curve.
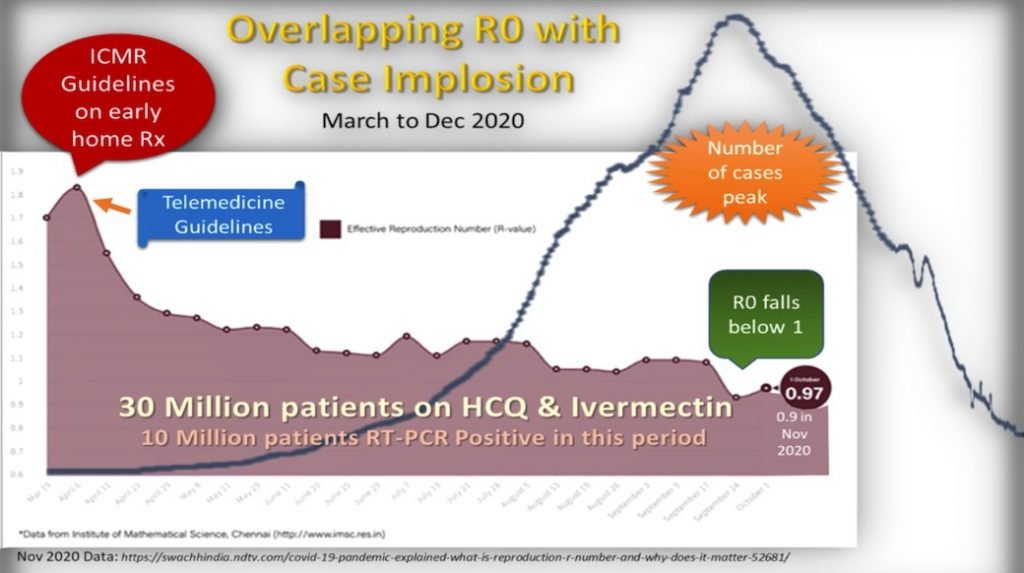
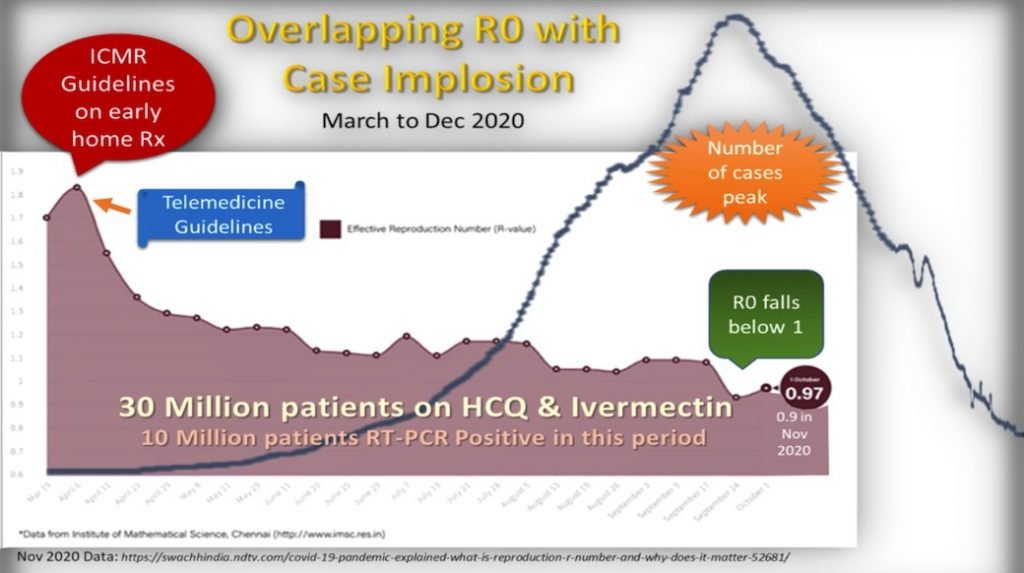
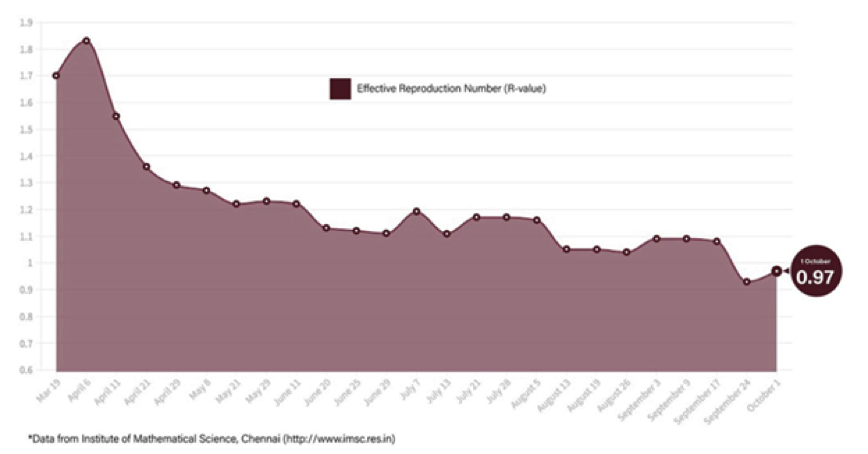
Herd Immunity Also called as “population immunity” is known to have occurred when a sufficient proportion of a population is immune to an infectious disease through vaccination or natural infection to reduce its spread within the community. As a result, even individuals not vaccinated (or infected) are offered protection as the disease has little opportunity to spread to the naïve, breaking the chain of transmission. This can be tested through serological surveys measuring antibodies in a cross section of people in certain geography to see what percentage of population has been exposed to the coronavirus, without developing symptoms. Such percentages have varied from 20% to 50% but not crossed 60% threshold which is said to be required for reaching herd immunity. However, an important epidemiological aspect has been ignored in this discussion. The threshold for herd immunity is not a fixed percentage but variable depending on the transmissibility of the virus in a community. Herd immunity threshold depends on R0, (R naught) which was near 2 in the early phase of transmission in India (Mar/Apr 2020) but fell dramatically in the next few months & subsequently reduced to lower than 1 in the month of Sept 2020 as shown in the graph below.
As seen from this graph, the R0 value (basic reproduction number i.e. the average number of people who will contract the disease from one infected person) in India has been on a steady decline; indicating a decrease in the rate of spread of the disease. When R0 falls below 1, each infected person will (technically) infect less than one person. At this rate, the disease eventually dies out. To confirm that R0<1 means achieving of herd immunity, we can mathematically calculate using the following formula to estimate the threshold; 1-1/R0. In this case 1-1/0.97 = -0.03 (negative 3% instead of positive 60% for R0 of 2.5).
What did India do differently to reduce R0?
It is eye-opening to explore as to how this happened in India but not in other countries where multiple waves kept coming within the same community despite country lockdowns. Let’s take the US and UK as examples. Both countries focused mainly on preventing the spread of the virus and took measures accordingly. Their home treatment guidelines for asymptomatic cases were to wait for 14 days in home isolation and for mild cases were to treat the symptoms with regular available medicines like vitamins and minerals. India, on the other hand, had a daunting challenge with the high population density, and inadequate testing and healthcare facilities in the initial stages. India had just 14 testing laboratories for Covid-19 in February 2020 which was increased to nearly 1600 by August 2020. The contact tracing efforts were ramped up and contacts were aggressively followed-up to ensure an almost complete coverage of cases. Considering the burden on hospitals, the decision was made to treat the asymptomatic and mild cases at home and moderate and severe cases in the hospitals.
Hence the ICMR recommended treatments came in handy for early treatment of patients at home. Since the country was in a lockdown, it was necessary to provide telemedicine guidelines for people to consult their primary care physicians on phone. Health ministry then simplified and liberalized their telemedicine guidelines in late March to suit the new model. These interventions occurred right from the first few months leading to R0 falling from April itself as seen from the graph on the previous page.
Proactive Aggressive treatment vs Reactive Hospitalizations:
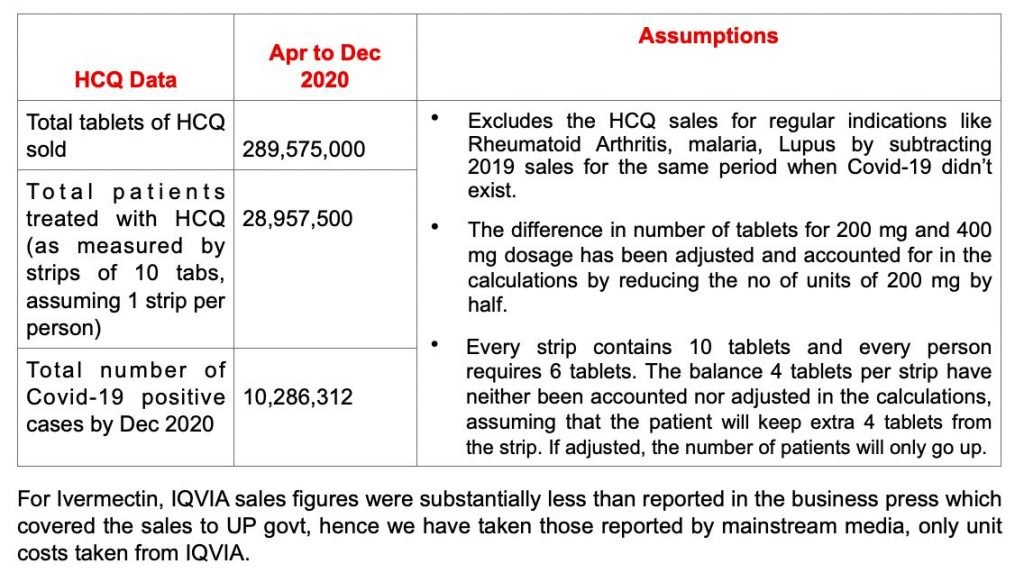
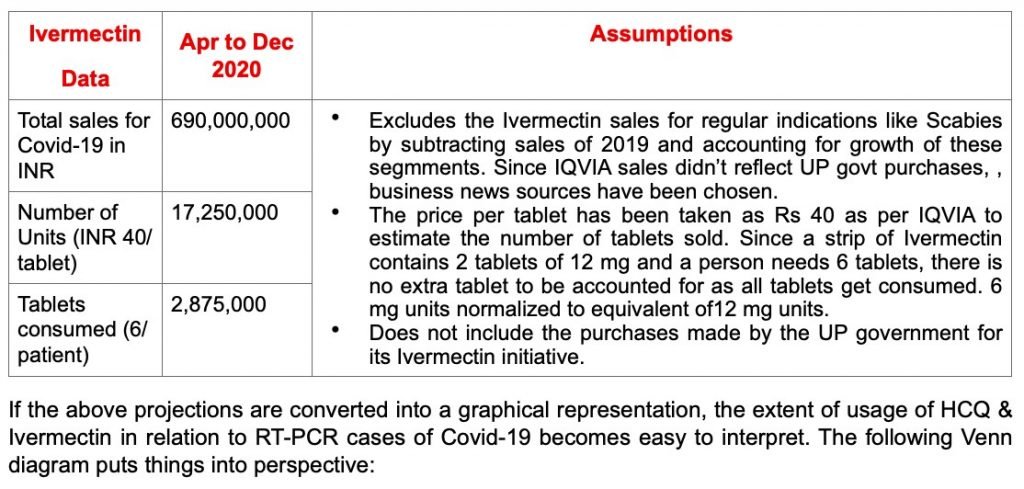
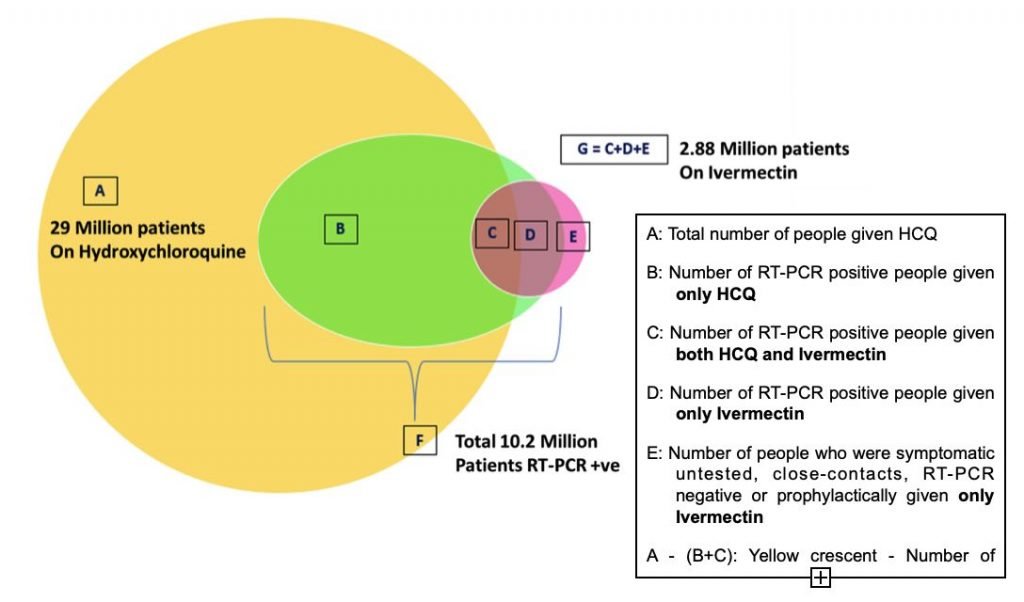
Could the aggressive first line treatment as per ICMR guidelines have slowed the spread of infection? To check this out we turned to the sales of HCQ (Hydroxychloroquine) during this period as it was recommended by the government. If we could convert the units into number of patients being treated and compare to the prevalence of Covid-19, we could get some correlation. Though not in the ICMR guidelines, we decided to add Ivermectin as the most populous state of UP declared to use it on a large scale in govt health centers.
Sales of Hydroxychloroquine and Ivermectin in India to project number of patients:
A compilation of HCQ data based on IQVIA sales figures (in addition to govt sales as reported in the press) for the period of April 2020 to December 2020 to project number of patients having received it.
Interpretation:
- It appears that 29 Mil. patients have received HCQ during the period of Mar-Dec 2020.
- Overlapping with these 29 Mil, 10.2 Mil pts were PCR +ve cases (or part of it) indicating that behind every +ve case around 2 more -ve patients have also been treated with HCQ. These could be either close contacts, untested or prophylaxis users.
- Patients taking Ivermectin is 56% of the RT-PCR positive cases. However, like the state of UP which replaced HCQ with Ivermectin, we have assumed only a 50% overlap with HCQ increasing the number of patients receiving either drugs.
- This would project the number of patients receiving either HCQ or Ivermectin to over 30 Mil (29 Mil + half of 5.75 Mil)
Thus, it is safe to assume that behind every positive case of Covid-19 in India, there were 2 more who received either HCQ or Ivermectin.
If we plot the R0 numbers along with the case devolution together with important milestones time-stamped together, the entire picture is clear from the following single graph, which doesn’t leave anything to imagination.
Limitation of the above data:
Due to the hype around HCQ & Ivermectin, it is possible that some portion of sales could be due to the stockpiling of these drugs at home/ by organizations etc. say around 10%. Even if the above projections are reduced by 10% it remains at 27 Million with a ratio of 2.7:1 usage indicating overuse beyond positive cases.
These numbers reflect an approach of aggressive early treatment of mild/moderate cases using the above 2 drugs going beyond PCR +ve cases. When correlated to the fall of R0 that led to the drop in new cases month to month seems to have played a major role in the control in India. These interventions could very well precipitate early reaching of herd immunity in India.
Conflict of Interest: Authors of this article work for an Indian big pharma which doesn’t sell either HCQ or Ivermectin in the Indian market, though it exports HCQ to US where it doesn’t have an EUA for Covid-19.
Authors: Dr. Pranit Desai, Mr. Preetam Chavan, Dr. Kshipra Gharpure, Dr. Chitra Bargaje & Dr. Dhananjay Bakhle ; Data reviewed by: Dr. Kishore Sonkusare
Sources:
- https://www.thehindubusinessline.com/news/by-september-india-could-have-111-crore-covid-19-cases-cddep/article31408132.ece
- https://www.npr.org/sections/goatsandsoda/2021/02/01/962821038/the-mystery-of-indias-plummeting-covid-19-cases
- https://news.yahoo.com/indias-sudden-drop-coronavirus-cases-212312608.html
- https://theprint.in/health/what-are-covid-mutations-in-india-are-they-more-infectious-gene-sequencing-has-the-answers/533203/
- https://www.hindustantimes.com/health/d614g-scientists-dispel-coronavirus-mutation-fears-say-10-times-more-infectious-malaysia-strain-no-cause-for-concern/story-Q5N0b1ItRnGTihGC3ZyVnI.html
- How to look after yourself at home if you have coronavirus (COVID-19) – NHS (www.nhs.uk)
- Treating COVID-19 at home: Care tips for you and others – Mayo Clinic
- https://www.mohfw.gov.in/pdf/UpdatedClinicalManagementProtocolforCOVID19dated03072020.pdf
- https://theprint.in/health/india-sold-over-22-crore-hcq-tablets-in-last-3-months-against-24-crore-in-all-of-2019/443587/
- https://www.business-standard.com/article/companies/sales-of-ivermectin-drug-to-treat-parasitic-infections-jump-fourfold-121020600005_1.html
- https://www.hindustantimes.com/india-news/ivermectin-not-to-be-included-in-centre-s-coronavirus-management-protocol/story-H2ahRiDO3nvCqktOBJGPjP.html
.png)

.png)





.jpg)
Comments
Post a Comment