How Does Orthopedic Surgery Stack Up to Interventional Orthobiologics?
One of the things that orthopedic surgery suffers from is that the basic technology is decades old and came into being at a time when there were very low research standards for surgical care. Take for example a knee replacement. If this procedure didn’t exist and I were to propose to the FDA and insurance companies today that I wanted to amputate a major part of someone’s body and insert a metal and plastic replacement, both would require large randomized controlled trials and a decade of research before allowing this to be approved and covered. Despite that, it took decades before someone tested a knee replacement against conservative care. Why is that a big deal? Because we didn’t know until that study that whacking out someone’s knee joint and replacing it with a prosthesis was better than going to physical therapy. In addition, we still don’t have a single study that compares a knee replacement to a placebo procedure (the medical term is sham). Why is that critical? Because the placebo effect of major surgery is HUGE.
On the other hand, any new therapy coming into being in the 21st century has been placed through a comparative research gauntlet. Randomized controlled trials are required to even have the conversation of whether something can get insurance coverage. Hence, regenerative medicine has had to move quickly into higher-level research that often exceeds the research base for the procedures being replaced. For example, while it took almost half a century for someone to publish a single RCT on knee replacement versus conservative care, a single decade has passed since providers began using PRP to treat knee arthritis and now we have more than two dozen randomized controlled trials showing it’s efficacy.
The UK Study
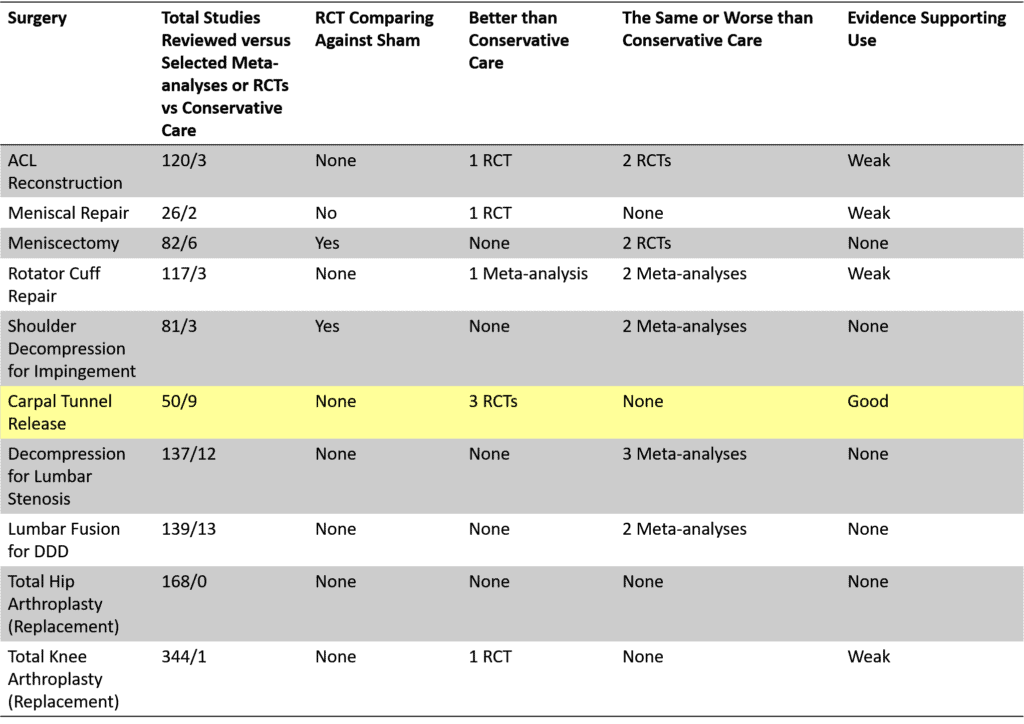
You probably remember this graph from a few weeks ago. It’s from a UK study that reviewed hundreds of high-level studies on orthopedic surgery to find the handful that actually compared surgery to conservative care or placebo (1). Meaning that there is no scientific rationale for pulling the trigger on an invasive surgery if there is no data showing that the surgery is better than something less invasive or doing nothing. This meta-analysis concluded that 9/10 of the most common orthopedic surgeries in use today had no basic scientific evidence that they are effective.
A colleague asked the interesting question last week of how Interventional Orthopedics would stack up? More on that below.
First, what is Interventional Orthopedics (aka Interventional Orthobiologics)? These are procedures that use precise image-guided platelet-rich plasma (PRP) and bone marrow concentrate (BMC) injections to help heal or manage orthopedic tissue damage. There are other things that can be injected as well and they often replace the need for invasive orthopedic surgery. Hence, it’s reasonable to ask how they stack up using the same 10 clinical conditions listed above.
For this review, I searched the US National Library of Medicine for the same diagnoses being treated above for randomized controlled trials (RCTs) comparing PRP or BMC to conservative care or placebo (2-41). I tried to match (as best I could) the same clinical indications that prompt the surgeries in the above table. In some instances (like rotator cuff tear), that only a partial match as that surgery can be performed for anything from massive to partial tears and massive tears are not candidates for PRP or BMC injection. This data produced this new table:
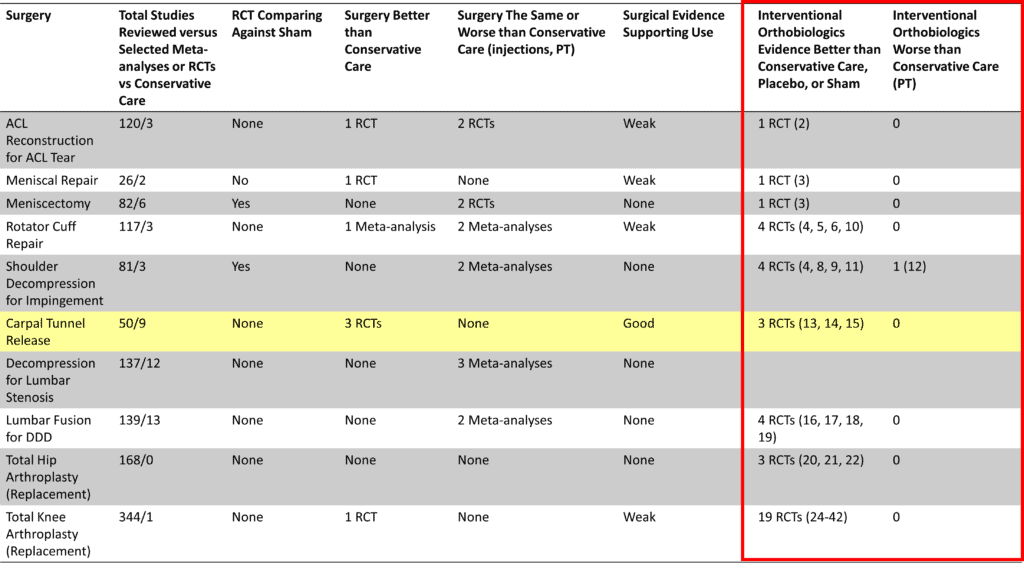
The two new columns are off on the right in the red box. Notice that there are generally more RCTs for Interventional Orthopedics (IO) procedures than the surgical column entitled “Surgery Better than Conservative Care”. Hence, it’s not hard to conclude that IO is killing it versus surgery.
Let’s take the example of knee replacement. We have one RCT showing that knee replacement is better than physical therapy, but NONE showing it’s better than a faked placebo procedure. On the IO side, we have about two dozen RCTs that show that PRP works to treat knee arthritis against placebo and various other injection treatments. We also have 3 RCTs that show that BMC injections are effective when compared to knee replacement or physical therapy. Again, because IO is newer, its basic evidence base is BETTER than surgery.
Where Could This Head?
I really think that in another 5 years that the evidence base supporting IO therapies could be so much better than surgery that national health systems and insurers could make a legitimate scientific argument that they need to start limiting coverage for orthopedic surgery in certain clinical situations in favor of Interventional Orthopedics. Meaning if I were an orthopedic surgeon, I would be concerned and pushing my colleagues to perform more basic studies versus conservative care.
The upshot? IO compares favorably to and in many instances beats the pants off of the basic science behind orthopedic surgery. Given that many of these PRP and BMC RCTs have been published in the past 12 months and that they are coming at a furious pace right now, the evidence base supporting IO is strong and getting stronger every month. I wish I could say the same about orthopedic surgery.
____________________________________________
References:
- Blom AW, Donovan RL, Beswick AD, Whitehouse MR, Kunutsor SK. Common elective orthopaedic procedures and their clinical effectiveness: umbrella review of level 1 evidence. BMJ. 2021 Jul 7;374:n1511. doi: 10.1136/bmj.n1511. PMID: 34233885.
- Centeno et al. Submitted for publication.
- Kaminski R, Maksymowicz-Wleklik M, Kulinski K, Kozar-Kaminska K, Dabrowska-Thing A, Pomianowski S. Short-Term Outcomes of Percutaneous Trephination with a Platelet Rich Plasma Intrameniscal Injection for the Repair of Degenerative Meniscal Lesions. A Prospective, Randomized, Double-Blind, Parallel-Group, Placebo-Controlled Study. Int J Mol Sci. 2019 Feb 16;20(4):856. doi: 10.3390/ijms20040856. PMID: 30781461; PMCID: PMC6412887.
- Kwong CA, Woodmass JM, Gusnowski EM, Bois AJ, Leblanc J, More KD, Lo IKY. Platelet-Rich Plasma in Patients With Partial-Thickness Rotator Cuff Tears or Tendinopathy Leads to Significantly Improved Short-Term Pain Relief and Function Compared With Corticosteroid Injection: A Double-Blind Randomized Controlled Trial. Arthroscopy. 2021 Feb;37(2):510-517. doi: 10.1016/j.arthro.2020.10.037. Epub 2020 Oct 28. PMID: 33127554.
- Jo CH, Lee SY, Yoon KS, Oh S, Shin S. Allogeneic Platelet-Rich Plasma Versus Corticosteroid Injection for the Treatment of Rotator Cuff Disease: A Randomized Controlled Trial. J Bone Joint Surg Am. 2020 Dec 16;102(24):2129-2137. doi: 10.2106/JBJS.19.01411. PMID: 33044249.
- Centeno C, Fausel Z, Stemper I, Azuike U, Dodson E. A Randomized Controlled Trial of the Treatment of Rotator Cuff Tears with Bone Marrow Concentrate and Platelet Products Compared to Exercise Therapy: A Midterm Analysis. Stem Cells Int. 2020 Jan 30;2020:5962354. doi: 10.1155/2020/5962354. PMID: 32399045; PMCID: PMC7204132.
- Schwitzguebel AJ, Kolo FC, Tirefort J, Kourhani A, Nowak A, Gremeaux V, Saffarini M, Lädermann A. Efficacy of Platelet-Rich Plasma for the Treatment of Interstitial Supraspinatus Tears: A Double-Blinded, Randomized Controlled Trial. Am J Sports Med. 2019 Jul;47(8):1885-1892. doi: 10.1177/0363546519851097. Epub 2019 Jun 4. PMID: 31161947.
- Dadgostar H, Fahimipour F, Pahlevan Sabagh A, Arasteh P, Razi M. Corticosteroids or platelet-rich plasma injections for rotator cuff tendinopathy: a randomized clinical trial study. J Orthop Surg Res. 2021 May 21;16(1):333. doi: 10.1186/s13018-021-02470-x. PMID: 34020672; PMCID: PMC8139041.
- Barreto RB, Azevedo AR, Gois MC, Freire MRM, Silva DS, Cardoso JC. Platelet-Rich Plasma and Corticosteroid in the Treatment of Rotator Cuff Impingement Syndrome: Randomized Clinical Trial. Rev Bras Ortop (Sao Paulo). 2019 Dec;54(6):636-643. doi: 10.1016/j.rboe.2018.03.002. Epub 2019 Dec 13. PMID: 31875061; PMCID: PMC6923638.
- Cai YU, Sun Z, Liao B, Song Z, Xiao T, Zhu P. Sodium Hyaluronate and Platelet-Rich Plasma for Partial-Thickness Rotator Cuff Tears. Med Sci Sports Exerc. 2019 Feb;51(2):227-233. doi: 10.1249/MSS.0000000000001781. PMID: 30199423; PMCID: PMC6336488.
Damjanov N, Barac B, Colic J, Stevanovic V, Zekovic A, Tulic G. The efficacy and safety of autologous conditioned serum (ACS) injections compared with betamethasone and placebo injections in the treatment of chronic shoulder joint pain due to supraspinatus tendinopathy: a prospective, randomized, double-blind, controlled study. Med Ultrason. 2018 Aug 30;20(3):335-341. doi: 10.11152/mu-1495. PMID: 30167587. - Nejati P, Ghahremaninia A, Naderi F, Gharibzadeh S, Mazaherinezhad A. Treatment of Subacromial Impingement Syndrome: Platelet-Rich Plasma or Exercise Therapy? A Randomized Controlled Trial. Orthop J Sports Med. 2017 May 19;5(5):2325967117702366. doi: 10.1177/2325967117702366. PMID: 28567426; PMCID: PMC5439655.
- Chen SR, Shen YP, Ho TY, Li TY, Su YC, Chou YC, Chen LC, Wu YT. One-Year Efficacy of Platelet-Rich Plasma for Moderate-to-Severe Carpal Tunnel Syndrome: A Prospective, Randomized, Double-Blind, Controlled Trial. Arch Phys Med Rehabil. 2021 May;102(5):951-958. doi: 10.1016/j.apmr.2020.12.025. Epub 2021 Feb 3. PMID: 33548206.
- Malahias MA, Nikolaou VS, Johnson EO, Kaseta MK, Kazas ST, Babis GC. Platelet-rich plasma ultrasound-guided injection in the treatment of carpal tunnel syndrome: A placebo-controlled clinical study. J Tissue Eng Regen Med. 2018 Mar;12(3):e1480-e1488. doi: 10.1002/term.2566. Epub 2017 Dec 17. PMID: 28873284.
- Wu YT, Ho TY, Chou YC, Ke MJ, Li TY, Huang GS, Chen LC. Six-month efficacy of platelet-rich plasma for carpal tunnel syndrome: A prospective randomized, single-blind controlled trial. Sci Rep. 2017 Dec;7(1):94. doi: 10.1038/s41598-017-00224-6. Epub 2017 Mar 7. PMID: 28273894; PMCID: PMC5427966.
- Ruiz-Lopez R, Tsai YC. A Randomized Double-Blind Controlled Pilot Study Comparing Leucocyte-Rich Platelet-Rich Plasma and Corticosteroid in Caudal Epidural Injection for Complex Chronic Degenerative Spinal Pain. Pain Pract. 2020 Jul;20(6):639-646. doi: 10.1111/papr.12893. Epub 2020 May 6. PMID: 32255266.
- Xu Z, Wu S, Li X, Liu C, Fan S, Ma C. Ultrasound-Guided Transforaminal Injections of Platelet-Rich Plasma Compared with Steroid in Lumbar Disc Herniation: A Prospective, Randomized, Controlled Study. Neural Plast. 2021 May 27;2021:5558138. doi: 10.1155/2021/5558138. PMID: 34135954; PMCID: PMC8175124.
- Cheng J, Santiago KA, Nguyen JT, Solomon JL, Lutz GE. Treatment of symptomatic degenerative intervertebral discs with autologous platelet-rich plasma: follow-up at 5-9 years. Regen Med. 2019 Sep;14(9):831-840. doi: 10.2217/rme-2019-0040. Epub 2019 Aug 29. PMID: 31464577; PMCID: PMC6770415.
- Wu J, Zhou J, Liu C, Zhang J, Xiong W, Lv Y, Liu R, Wang R, Du Z, Zhang G, Liu Q. A Prospective Study Comparing Platelet-Rich Plasma and Local Anesthetic (LA)/Corticosteroid in Intra-Articular Injection for the Treatment of Lumbar Facet Joint Syndrome. Pain Pract. 2017 Sep;17(7):914-924. doi: 10.1111/papr.12544. Epub 2017 Feb 22. PMID: 27989008.
- Dallari D, Stagni C, Rani N, Sabbioni G, Pelotti P, Torricelli P, Tschon M, Giavaresi G. Ultrasound-Guided Injection of Platelet-Rich Plasma and Hyaluronic Acid, Separately and in Combination, for Hip Osteoarthritis: A Randomized Controlled Study. Am J Sports Med. 2016 Mar;44(3):664-71. doi: 10.1177/0363546515620383. Epub 2016 Jan 21. PMID: 26797697.
- Kraeutler MJ, Houck DA, Garabekyan T, Miller SL, Dragoo JL, Mei-Dan O. Comparing Intra-articular Injections of Leukocyte-Poor Platelet-Rich Plasma Versus Low-Molecular Weight Hyaluronic Acid for the Treatment of Symptomatic Osteoarthritis of the Hip: A Double-Blind, Randomized Pilot Study. Orthop J Sports Med. 2021 Jan 20;9(1):2325967120969210. doi: 10.1177/2325967120969210. PMID: 33786329; PMCID: PMC7934058.
- Villanova-López MM, Núñez-Núñez M, Fernández-Prieto D, González-López C, García-Donaire J, Pérez-Pérez A, Sandoval Fernández Del Castillo S, Murillo-Izquierdo M, Camean-Fernández M, Gutiérrez-Pizarraya A, Navas-Iglesias N, Roca-Ruiz LJ, Calleja-Hernández MÁ, Ballester-Alfaro JJ. Randomized, double-blind, controlled trial, phase III, to evaluate the use of platelet-rich plasma versus hyaluronic acid in hip coxarthrosis. Rev Esp Cir Ortop Traumatol (Engl Ed). 2020 Mar-Apr;64(2):134-142. English, Spanish. doi: 10.1016/j.recot.2019.09.008. Epub 2020 Jan 2. PMID: 31902736.
- Di Sante L, Villani C, Santilli V, Valeo M, Bologna E, Imparato L, Paoloni M, Iagnocco A. Intra-articular hyaluronic acid vs platelet-rich plasma in the treatment of hip osteoarthritis. Med Ultrason. 2016 Dec 5;18(4):463-468. doi: 10.11152/mu-874. PMID: 27981279. (5) Uslu Güvendi E, Aşkin A, Güvendi G, Koçyiğit H. Comparison of Efficiency Between Corticosteroid and Platelet Rich Plasma Injection Therapies in Patients With Knee Osteoarthritis. Arch Rheumatol. 2017;33(3):273–281. Published 2017 Nov 2. doi: 10.5606/ArchRheumatol.2018.6608
- Tavassoli M, Janmohammadi N, Hosseini A, Khafri S, Esmaeilnejad-Ganji SM. Single- and double-dose of platelet-rich plasma versus hyaluronic acid for treatment of knee osteoarthritis: A randomized controlled trial. World J Orthop. 2019;10(9):310–326. Published 2019 Sep 18. doi: 10.5312/wjo.v10.i9.310
- Joshi Jubert N, Rodríguez L, Reverté-Vinaixa MM, Navarro A. Platelet-Rich Plasma Injections for Advanced Knee Osteoarthritis: A Prospective, Randomized, Double-Blinded Clinical Trial. Orthop J Sports Med. 2017;5(2):2325967116689386. Published 2017 Feb 13. doi: 10.1177/2325967116689386
- Raeissadat SA, Rayegani SM, Hassanabadi H, et al. Knee Osteoarthritis Injection Choices: Platelet- Rich Plasma (PRP) Versus Hyaluronic Acid (A one-year randomized clinical trial). Clin Med Insights Arthritis Musculoskelet Disord. 2015;8:1–8. Published 2015 Jan 7. doi: 10.4137/CMAMD.S17894
- Montañez-Heredia E, Irízar S, Huertas PJ, et al. Intra-Articular Injections of Platelet-Rich Plasma versus Hyaluronic Acid in the Treatment of Osteoarthritic Knee Pain: A Randomized Clinical Trial in the Context of the Spanish National Health Care System. Int J Mol Sci. 2016;17(7):1064. Published 2016 Jul 2. doi: 10.3390/ijms17071064
- Görmeli G, Görmeli CA, Ataoglu B, Çolak C, Aslantürk O, Ertem K. Multiple PRP injections are more effective than single injections and hyaluronic acid in knees with early osteoarthritis: a randomized, double-blind, placebo-controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017 Mar;25(3):958-965. doi: 10.1007/s00167-015-3705-6.
- Lana JF, Weglein A, Sampson SE, et al. Randomized controlled trial comparing hyaluronic acid, platelet-rich plasma and the combination of both in the treatment of mild and moderate osteoarthritis of the knee. J Stem Cells Regen Med. 2016;12(2):69–78. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5227106/
- Tavassoli M, Janmohammadi N, Hosseini A, Khafri S, Esmaeilnejad-Ganji SM. Single- and double-dose of platelet-rich plasma versus hyaluronic acid for treatment of knee osteoarthritis: A randomized controlled trial. World J Orthop. 2019;10(9):310–326. Published 2019 Sep 18. doi: 10.5312/wjo.v10.i9.310
- Lin KY, Yang CC, Hsu CJ, Yeh ML, Renn JH. Intra-articular Injection of Platelet-Rich Plasma Is Superior to Hyaluronic Acid or Saline Solution in the Treatment of Mild to Moderate Knee Osteoarthritis: A Randomized, Double-Blind, Triple-Parallel, Placebo-Controlled Clinical Trial. Arthroscopy. 2019 Jan;35(1):106-117. doi: 10.1016/j.arthro.2018.06.035.
- Huang Y, Liu X, Xu X, Liu J. Intra-articular injections of platelet-rich plasma, hyaluronic acid or corticosteroids for knee osteoarthritis : A prospective randomized controlled study. Orthopade. 2019 Mar;48(3):239-247. doi: 10.1007/s00132-018-03659-5.
- Di Martino A, Di Matteo B, Papio T, Tentoni F, Selleri F, Cenacchi A, Kon E, Filardo G. Platelet-Rich Plasma Versus Hyaluronic Acid Injections for the Treatment of Knee Osteoarthritis: Results at 5 Years of a Double-Blind, Randomized Controlled Trial. Am J Sports Med. 2019 Feb;47(2):347-354. doi: 10.1177/0363546518814532.
- Yu W, Xu P, Huang G, Liu L. Clinical therapy of hyaluronic acid combined with platelet-rich plasma for the treatment of knee osteoarthritis. Exp Ther Med. 2018;16(3):2119–2125. doi: 10.3892/etm.2018.6412
- Buendía-López D, Medina-Quirós M, Fernández-Villacañas Marín MÁ. Clinical and radiographic comparison of a single LP-PRP injection, a single hyaluronic acid injection and daily NSAID administration with a 52-week follow-up: a randomized controlled trial. J Orthop Traumatol. 2018;19(1):3. Published 2018 Aug 20. doi: 10.1186/s10195-018-0501-3
- Su K, Bai Y, Wang J, Zhang H, Liu H, Ma S. Comparison of hyaluronic acid and PRP intra-articular injection with combined intra-articular and intraosseous PRP injections to treat patients with knee osteoarthritis. Clin Rheumatol. 2018 May;37(5):1341-1350. doi: 10.1007/s10067-018-3985-6.
- Louis ML, Magalon J, Jouve E, Bornet CE, Mattei JC, Chagnaud C, Rochwerger A, Veran J3, Sabatier F. Growth Factors Levels Determine Efficacy of Platelets Rich Plasma Injection in Knee Osteoarthritis: A Randomized Double Blind Noninferiority Trial Compared With Viscosupplementation. Arthroscopy. 2018 May;34(5):1530-1540.e2. doi: 10.1016/j.arthro.2017.11.035.
- Lisi C, Perotti C, Scudeller L, Sammarchi L, Dametti F, Musella V, Di Natali G. Treatment of knee osteoarthritis: platelet-derived growth factors vs. hyaluronic acid. A randomized controlled trial. Clin Rehabil. 2018 Mar;32(3):330-339. doi: 10.1177/0269215517724193
- Cole BJ, Karas V, Hussey K, Pilz K, Fortier LA. Hyaluronic Acid Versus Platelet-Rich Plasma: A Prospective, Double-Blind Randomized Controlled Trial Comparing Clinical Outcomes and Effects on Intra-articular Biology for the Treatment of Knee Osteoarthritis. Am J Sports Med. 2017 Feb;45(2):339-346. doi: 10.1177/0363546516665809.
- Centeno C, Sheinkop M, Dodson E, et al. A specific protocol of autologous bone marrow concentrate and platelet products versus exercise therapy for symptomatic knee osteoarthritis: a randomized controlled trial with 2 year follow-up. J Transl Med. 2018;16(1):355. doi:10.1186/s12967-018-1736-8
- Hernigou P, Bouthors C, Bastard C, Flouzat Lachaniette CH, Rouard H, Dubory A. Subchondral bone or intra-articular injection of bone marrow concentrate mesenchymal stem cells in bilateral knee osteoarthritis: what better postpone knee arthroplasty at fifteen years? A randomized study. Int Orthop. 2020 Jul 2. doi: 10.1007/s00264-020-04687-7. Epub ahead of print. PMID: 32617651.
- Hernigou P, Delambre J, Quiennec S, Poignard A. Human bone marrow mesenchymal stem cell injection in subchondral lesions of knee osteoarthritis: a prospective randomized study versus contralateral arthroplasty at a mean fifteen year follow-up. Int Orthop. 2020 Apr 23. doi: 10.1007/s00264-020-04571-4. Epub ahead of print. PMID: 32322943.
.png)

.png)






Comments
Post a Comment