FDA Proposal on Salt Substitutes May Bring Unexpected Harms
The Food and Drug Administration’s drive toward salt substitutes, aimed at reducing dietary sodium, faces mounting skepticism from top health experts.
Salt has been in the FDA’s crosshairs for some time. Since October 2021, the federal agency has notably urged restaurants and food manufacturers to take voluntary measures to reduce salt use, targeting reductions in sodium across more than 160 food categories.
The FDA is advocating for a transition from traditional salt to potential lower-sodium alternatives, a notable deviation from prior guidelines, as outlined in its proposal, “Use of Salt Substitutes to Reduce the Sodium Content in Standardized Foods.”
FDA’s Salt Swap Initiative
The FDA is currently revising the “standards of identity”—essentially the official blueprints that determine the ingredients and processes required for a product to bear a specific label, such as “bread” or “mayonnaise.” With these updates, the agency proposes that certain foods can now include “safe and suitable” low-sodium salt alternatives, marking a shift from the traditionally stricter guidelines.
Explaining the motivation behind this move, FDA Commissioner Dr. Robert M. Califf emphasized the broader goal of enhanced nutrition and chronic disease reduction. “By providing manufacturers another tool to decrease sodium in food production, we aim to lower Americans’ risk of conditions such as hypertension, which is intrinsically linked to heart disease and stroke,” he stated in a press release in March 2023.
In response to the FDA’s proposal on salt substitutes, the International Food Additives Council (IFAC) and The Glutamate Association voiced support, underscoring potential benefits for food manufacturers and consumers. The IFAC emphasized flexibility in using salt alternatives. The Glutamate Association pointed to research from countries such as Japan and Brazil that showed glutamates and MSG can reduce sodium by as much as 50 percent in diverse cuisines without sacrificing flavor.
If the proposal moves forward, its impacts could reach every corner of our pantries. Everything from canned goods to the assortment of condiments, down to the very bread that we use for our sandwiches, might be affected by this guidance.
About 90 percent of Americans regularly surpass the suggested daily sodium limit, set at 2,300 milligrams, according to the Centers for Disease Control and Prevention (CDC). Sodium consumption by adults is 50 percent above this recommended limit, according an FDA report, which states that more than 70 percent of the nation’s sodium intake comes from manufactured and commercially prepared foods.Replace Salt With What?
Salt substitutes, such as Nu-Salt or Morton Salt Substitute, primarily contain ingredients that mimic the familiar salty taste without sodium. While sodium chloride forms the essence of regular table salt, these substitutes typically employ potassium chloride. However, some might blend in other components, such as herbs, spices, or amino acids.The FDA’s draft doesn’t pinpoint specific allowable substitutes but simply labels them as “safe and appropriate,” hinting at alternatives beyond potassium chloride.
“Other ingredients listed in the scientific literature include herbs and spices, yeast extracts, monosodium glutamate, amino acids, and dairy extracts,” the brief reads.
For an additive to make its way into our foods, it must either have FDA approval or be universally accepted as safe. Sodium chloride, our go-to table salt, effortlessly checks that box. But as these regulations evolve, the definition of a “salt substitute” might transform. These envisioned alternatives, which could be a single ingredient or a mix, must reduce sodium without sacrificing the food’s core flavor or safety—a challenge that manufacturers will have to address.Health Organizations Caution Against Salt Substitutes
The concerns revolve around the potential health risks to the 37 million Americans who have been diagnosed with chronic kidney disease (CKD). Many CKD patients, they note, are unable to adequately process excess potassium, making them susceptible to hyperkalemia, a dangerous condition that can lead to severe cardiac complications and even sudden death.
While these organizations laud the FDA’s efforts to mitigate the high sodium consumption among Americans, they stress the need for a more cautious approach. The letter pointedly highlights that adding “hidden potassium” in foods, especially without clear labeling, could inadvertently imperil a significant portion of the population.
Potassium—crucial for muscle contraction, especially in the heart—must be carefully balanced. When this balance is disrupted, it can cause muscle malfunction, including in the heart. While kidneys manage about 80 percent of the potassium that we consume, other organs such as the adrenal glands and pancreas, as well as many medications, can also affect potassium levels.
Dr. Stephen Z. Fadem, chair of AAKP’s Medical Advisory Board and clinical professor of medicine at Baylor College of Medicine, cautions against unchecked potassium in food products. “If potassium is indiscriminately added to foods, it will result in many patients ingesting more than their body can handle. This is ill-advised and against the U.S. FDA’s mission of shepherding safe and effective care,” he told The Epoch Times.
The letter further warns that the dangers extend beyond those with kidney disease. “Other populations vulnerable to excessive potassium and associated health risks, because they too are unable to normally excrete it, include those with heart failure, diabetes, adrenal insufficiency, and those taking medications that impair potassium excretion.”
The letter strongly urges the FDA to pivot toward alternate strategies in light of these potential health ramifications. This could include developing flavor enhancers that aren’t potassium-based, intensifying public health education about safe sodium reduction, or enhancing food labeling. The collective plea underscores the need for both public safety and transparent communication in any forthcoming regulatory changes.
Paul Conway, AAKP’s chair of policy and global affairs, highlighted the significant impacts of kidney disease on patients and the economy.
“Kidney disease is a health care and workforce issue because of the amount of disability it can create. Beyond the personal toll on patients and their families, it’s a financial strain, costing America $130 billion a year for kidney care. This figure doesn’t even account for the repercussions of disability, job loss, and unemployment due to the disease,” he told The Epoch Times.
Mr. Conway also took issue with the FDA’s approach to formulating its proposal, noting that crucial organizations, such as his own, were sidelined from the outset, leading to a policy with unintended consequences.
“We should have been at the forefront of this policy. If you release regulations for public comment and are met with surprise feedback, you’ve gone about it wrong. We don’t always weigh in on such matters. When we do, our voice carries significant weight due to the severity of the disease we address and its associated mortality rates,” he said.
The American Diabetes Association and the American College of Cardiology didn’t respond to requests for comment.The Great Salt Debate
Salt—essential for our bodily functions—has long been a topic of debate among health experts.
The National Institutes of Health brought salt into sharp focus in 2001 with the DASH-sodium study, suggesting a connection between reduced sodium consumption and decreased blood pressure that led to salt’s cautionary positioning in America’s dietary guidelines.
Despite significant investments in research, definitive evidence remains hard to come by. The central question revolves around whether prolonged high salt intake, culminating in hypertension, ultimately escalates to graver health complications.
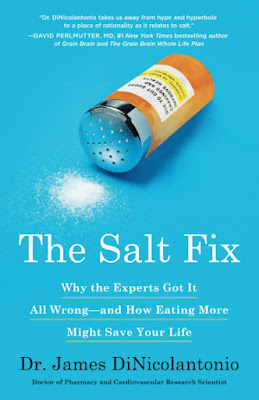
James DiNicolantonio, a cardiovascular research scientist and author of “The Salt Fix,” offers a critical perspective on this issue.
“It’s more than likely that replacing nature’s oldest food preservative and essential mineral with a salt substitute will lead to more harm than good and unintended consequences, such as kids no longer eating their bitter vegetables, eggs or meat because there’s no salt (flavor) to go with it and now consuming more refined carbohydrates and refined sugars,” he said.\
“Additionally, when it comes to storing food, low salt versions dramatically increase food spoilage (they don’t last as long) and food borne illness.”
In a comprehensive study of more than 28,000 high-risk individuals, researchers found a nuanced relationship between sodium and heart health. Elevated sodium levels were linked to a rise in cardiovascular risks. Surprisingly, however, very low intakes were associated with an increased likelihood of cardiovascular mortality.
Adding complexity, a 2023 investigation revealed that heart failure patients who were consuming less than 2.5 grams of sodium daily faced an 80 percent heightened mortality risk compared to their counterparts.
“Our findings showed that restricting dietary sodium below recommended levels was counterproductive in managing heart failure,” Dr. Anirudh Palicherla, the study’s lead researcher, stated. It’s important to identify a safe sodium consumption level, he said.
Mr. DiNicolantonio further adds to the salt debate, saying, “There is no proof that lowering sodium intake will lead to definitive improvements in high blood pressure, target organ function, strokes, heart attacks, etc. Salt is an essential mineral and the body can’t make it.”
Andrew Huberman, a neurobiology professor at Stanford University School of Medicine, highlights sodium’s pivotal role in cognitive and physical well-being. “I want to emphasize the possibility, that for some people, more salt might help them in terms of health, cognitive, and bodily functioning, and for other people, less salt is going to be better,” he commented in a recent podcast episode.
It’s worth noting that not all salt is created equal, recent research suggests. In a Stanford University study, rats fed natural sea salt displayed consistently lower blood pressure and fewer cardiac and kidney issues than their counterparts on refined salt, suggesting that natural salts may have health benefits over their refined counterparts.
A Medical Perspective: Health Professional Weigh In
The call to cut sodium has sparked a spectrum of medical opinions. While many in the health care realm view this as an important step toward bolstering public health, the lurking hazards of high salt consumption remain ever-present.
“Lowering salt intake carries significant public health advantages, especially in reducing average blood pressure,” Dr. Richard J. Solomon, medical director of nephrology at the University of Vermont Medical Center, told The Epoch Times.
He underscores the urgent need for precise product labeling and robust public education. Dr. Solomon believes that labels should indicate if foods contain potassium chloride—an essential warning for those with kidney issues. He advises the public to “consult with a physician” before reaching for products laden with salt substitutes.
Nephrology specialist and dietician Desiree De Waal emphasizes the importance of clear labeling, akin to “added sugars.” However, she highlights pitfalls in potassium labeling. Labeling such as “good source of potassium” aids those with kidney ailments, but poses risks for the unaware.
“Those uninformed of their kidney disease risk hyperkalemia, which can lead to cardiac arrest. I’ve seen many patients misled by this, with dangerously high potassium levels resulting in hospitalizations,” Ms. De Waal told The Epoch Times.
She expressed concerns about the long-term risks of food additives, especially harmful preservatives such as phosphorus additives. “We need to focus on herbs and spices. Our salt-centric society has lost the authentic taste of food,” Ms. De Waal said.
Amid ongoing debates about salt substitutes, Dr. Fadem suggests a return to the basics.
“People who eat more fresh foods will not only be healthier but will not have to rely on salt substitutes for flavor,” he said.
This viewpoint underscores the idea that a return to natural, unprocessed foods may hold the key to navigating the contemporary salt dilemma, as well as the many health concerns tied to diets high in processed and ultra-processed foods.
According to Mr. DiNicolantonio: “The FDA needs to go after actual harmful substances like refined seed oils, refined sugars and processed junk food. Leave salt where it should be, on the kitchen table.”
Reposted from: https://www.theepochtimes.com/health/fda-proposal-on-salt-substitute-may-bring-unexpected-harms-5474969

.png)
.png)






Comments
Post a Comment