Cytokine Storm 101: Symptoms, Causes, Diagnosis and Treatment 2023
What Is Cytokine Storm?
Broadly speaking, cytokine storm is a cascade of exaggerated immune responses that can cause serious problems. The immune system contains many different components that help you battle infections. It includes many different types of cells that communicate with each other via signaling molecules, known as cytokines.
There are many different cytokines that perform many kinds of functions. Some
help recruit other immune cells, and some help with antibody production or
pain signaling. Some make the blood clot more easily. Some help produce
inflammation, which can make blood vessels more leaky than normal.
Another
group of cytokines helps tamp down the body’s inflammatory response. That’s an
important balance, since too much inflammation causes its own problems.
Under
normal circumstances, these cytokines help coordinate the response of your
immune system to take care of infectious substances, like viruses or bacteria.
The problem is that sometimes the body’s inflammatory response can get out of
control, causing more harm than good.
Sometimes the body produces too many inflammatory cytokines and not
enough cytokines that modulate inflammation. The inflammatory cytokines
start “storming” out of control, without enough feedback from the
anti-inflammatory cytokines.2
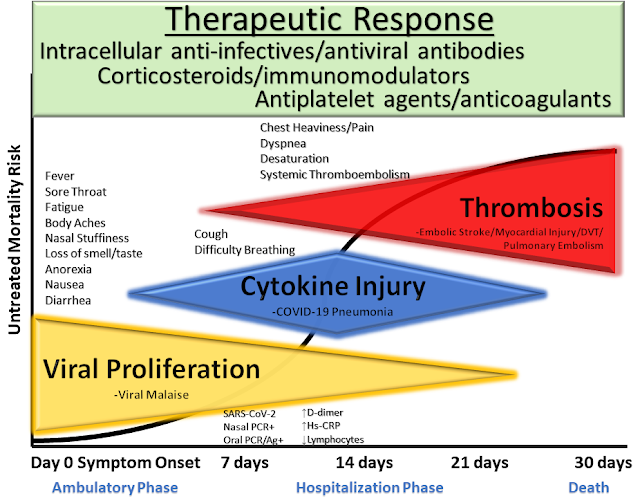
In people experiencing cytokine storm syndrome, certain cytokines are present in the blood at higher-than-normal amounts. In COVID-19, elevations in several inflammatory cytokines seem to be involved in the development of acute respiratory distress syndrome, the leading cause of death in people dealing with COVID-19 illness.3
Cytokine Storm Syndrome Symptoms
Cytokine storm can cause many different symptoms. Sometimes these are only mild, flu-like symptoms. Other times, these can be severe and life-threatening. Symptoms might include:4
- Fevers and chills
- Fatigue
- Swelling of extremities
- Nausea and vomiting
- Muscle and joint aches
- Headache
- Rash
- Cough
- Shortness of breath
- Rapid breathing
- Seizures
- Tremor
- Difficulty coordinating movements
- Confusion and hallucinations
- Lethargy and poor responsiveness
Very low blood pressure and increased blood clotting can also be hallmarks of severe cytokine storm syndrome. The heart may not pump as well as it normally would. As a result, cytokine storm can affect multiple organ systems, potentially leading to organ failure and death.5
Causes
Scientists are still working to understand the complex web of causes that can cause cytokine storm to start. It can be caused by several different types of underlying health issues.
Genetic Syndromes
People with certain genetic syndromes are predisposed to experiencing cytokine
storm. For example, this applies to people with a condition called familial
hemophagocytic lymphohistiocytosis (HLH). These genetic defects lead to
specific problems in certain immune system cells.
People who have a
genetic condition in this group are prone to developing cytokine storm in
response to infections, usually within the first few months of life.6
Infection
Certain types of infections can also trigger cytokine storm in some people, including those caused by viruses, bacteria, and other agents. One of the most commonly studied types is cytokine storm from influenza A virus (the virus that causes the common flu). Severe types of influenza infections may be more likely to cause cytokine storm.7
For example, it’s thought that cytokine storm syndrome might have been the reason for the high death rate in young adults during the 1918 influenza pandemic. Epstein-Barr virus and cytomegalovirus are some other common infectious causes.8
Even though most people don't experience cytokine storm, certain types of infections are more likely to cause it than others.
For reasons that aren’t yet completely clear, the SARS-CoV-2 virus that causes COVID-19 seems more prone to result in cytokine storm compared to diseases caused by some other viruses.3
That's a big reason why the virus poses such a worldwide problem.
Autoimmune disease
People with certain autoimmune syndromes have a higher risk of getting cytokine storm syndrome. For example, this can occur in Still’s disease, in systemic juvenile idiopathic arthritis (JIA), and in lupus. In this context, cytokine storm often goes by the name “macrophage activation syndrome.”8
This type of cytokine storm might occur when a person’s underlying disease is flaring up, or when the person is also experiencing some kind of infection.
Other Causes
Cytokine storm can also sometimes be a side effect of specific medical therapies. For example, it has sometimes occurred after a therapy for leukemia known as CAR-T therapy (chimeric antigen receptor T cells).9 Other types of immunotherapy have also sometimes caused cytokine storm as a side effect.
Cytokine storm can also occur in other medical situations, such as after receiving an organ or stem cell transplant. Certain types of cancers can also cause a cytokine storm syndrome, as can conditions that affect the immune system, like AIDS.10
Sepsis, a life-threatening immune response to an infection, is also sometimes broadly thought of as being a type of cytokine storm syndrome.11
COVID-19
Most people with COVID-19 do not develop cytokine storm and its symptoms. Certain people may be more prone to developing cytokine storm from COVID-19 if they have specific genes that make their immune system react in certain ways.2
At this point, this is not known for sure. Other factors, such as the presence of underlying health conditions, may be much bigger determinants of the severity of a COVID-19 infection.
Cytokine Storm Syndrome Diagnosis
Cytokine storm is diagnosed in the context of the underlying medical condition. This underlying problem might be already known, or it may require its own diagnosis.
A person might need to be diagnosed with a genetic disorder, autoimmune condition, or an infectious disease, like COVID-19. Depending on the situation, this might require various kinds of medical tests, like specific blood tests.
Medical history and physical exam provide diagnostic starting points. Your clinician will want to know about your past medical issues and recent symptoms.
The clinician will also thoroughly examine you for signs that might indicate cytokine storm. This is important, because cytokine storm can affect so many different systems of the body. Abnormally low blood pressure, fever, and low oxygen in the blood (hypoxia) might be found.
It’s important for clinicians to recognize that cytokine storm is a possibility, because it is such a dangerous condition.
Laboratory abnormalities, like may be seen in basic blood tests, can provide clues. People with cytokine storm might have abnormalities like the following:5
- Decreased number of immune cells
- Elevations in markers of kidney or liver damage
- Elevations in inflammatory markers like C-reactive protein (CRP)
- Abnormalities in markers of blood clotting
- Elevated ferritin (involved in infection response)
Medical imaging can also provide clues. For example, a chest X-ray might display lung involvement from cytokine storm related to COVID-19.
Researchers are working hard to understand what cytokine storm means in the context of COVID-19. Some clinicians have suggested screening patients with the disease for laboratory signs of inflammation that might indicate a cytokine storm, like elevated ferritin levels.12
It has been suggested that these individuals might benefit from therapies targeted to address cytokine storm and tamp down the immune system. However, this is not yet clear.
Treatment
Supportive care is a critical part of treatment for cytokine storm. If an individual is experiencing severe symptoms (like difficulty breathing), they may need care in an intensive care unit. This might include support such as the following:13
- Intensive monitoring of vital signs
- Ventilatory support
- Fluids given intravenously
- Management of electrolytes
- Hemodialysis
In some situations, it may be possible to treat the underlying source of the cytokine storm. For example, if cytokine storm is caused by a bacterial infection, an antibiotic may be helpful.
However, in many cases a direct treatment for the underlying condition is not available, and clinicians must try other approaches to try to decrease the immune response. But it is very complicated, in part because the immune system has so many different parts.
In fighting off an infection, it might be ideal to tone down one part of the immune response while leaving another part working normally, or even strengthening it.2
Many different therapies have been tried, but scientists do not currently agree about the best way to treat cytokine storm in all circumstances. The best options may depend somewhat on the specific underlying cause of the cytokine storm.
For example, corticosteroids seem to be very helpful for people with cytokine storm due to underlying autoimmune disease.8 However, it's not clear that this is the best option for people with cytokine storm from an infectious cause, like in COVID-19.
Timing may also be critical for effective therapy, since treatments that might be helpful early might not be effective later, and vice versa. There may also be a lot of variability in how people respond to such therapies.
In the past, some treatments have been tried for cytokine storm with some mixed success. These include:2
- Aspirin
- Corticosteroids
- Drugs that affect the immune system, like cyclosporine
- Biological therapies that block specific cytokines
- Plasma exchange (plasmapheresis)
- Statin drugs
Treatment of Cytokine Storm from COVID-19
Researchers are actively exploring many different therapies to treat cytokine storm syndrome from COVID-19. Many are studying existing therapies that affect the immune system to see if any might help people with cytokine storm from COVID-19.
For example, Kineret (anakinra) is a biologic therapy sometimes used to treat people with rheumatoid arthritis and other medical conditions that can affect the immune system. It blocks the activity of a specific cytokine known as interleukin 1 (IL-1). It has sometimes been helpful for people with cytokine storm from autoimmune conditions.8
Researchers are currently studying whether this therapy might help critically ill people with cytokine storm syndrome from COVID-19.
Another example is Actemra (tocilizumab), a biologic that can be used for rheumatoid arthritis and other conditions. This therapy blocks the activity of another cytokine, interleukin 6 (IL-6). Actemra has previously sometimes been used to treat cytokine storm resulting as a side effect of therapy (like for leukemia).4
Scientists are currently investigating these therapies, as well as many other potential interventions.14 Ideally, multiple therapies will be found to help curb the effects of cytokine storm, leading to decreased deaths from COVID-19.
FREQUENTLY ASKED QUESTIONS
What is hypercytokinemia?Hypercytokinemia is the medical term for cytokine storm. It refers to the overproduction of cytokines, certain proteins that send messages between cells. When the body loses control of cytokine production, their excessive numbers cause an internal response that resembles many infectious and non-infectious diseases.15
What are the symptoms of cytokine storm?
Symptoms of cytokine storm can range from mild, flu-like symptoms to severe and life-threatening complications. Examples include confusion, cough, fatigue, fever, issues with coordination, headache, lethargy, swelling of extremities, rapid breathing, seizures, and more.
Sources
- Guo YR, Cao QD, Hong ZS, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak--an update on the status. Mil Med Res. 2020;7(1):11. doi:10.1186/s40779-020-00240-0
- Tisoncik JR, Korth MJ, Simmons CP, et al. Into the eye of the cytokine storm. Microbiol Mol Biol Rev. 2012;76(1):16–32. doi:10.1128/MMBR.05015-11
- Ye Q, Wang B, Mao J. Cytokine storm in COVID-19 and treatment. J Infect. 2020 Apr 10. doi:10.1016/j.jinf.2020.03.037
- Lee DW, Gardner R, Porter DL, et al. Current concepts in the diagnosis and management of cytokine release syndrome. Blood. 2014;124(2):188–195. doi:10.1182/blood-2014-05-552729
- Shimabukuro-Vornhagen A, Gödel P, Subklewe M, et al. Cytokine release syndrome. J Immunother Cancer. 2018;6(1):56. doi:10.1186/s40425-018-0343-9
- Sieni E, Cetica V, Hackmann Y, et al. Familial hemophagocytic lymphohistiocytosis: when rare diseases shed light on immune system functioning. Front Immunol. 2014;5:167. doi:10.3389/fimmu.2014.00167
- D'Elia RV, Harrison K, Oyston PC, Lukaszewski RA, Clark GC. Targeting the "cytokine storm" for therapeutic benefit. Clin Vaccine Immunol. 2013;20(3):319–327. doi:10.1128/CVI.00636-12
- Schulert GS, Grom AA. Pathogenesis of macrophage activation syndrome and potential for cytokine- directed therapies. Annu Rev Med. 2015;66:145–159. doi:10.1146/annurev-med-061813-012806
- Grupp SA, Kalos M, Barrett D, et al. Chimeric antigen receptor-modified T cells for acute lymphoid leukemia. N Engl J Med. 2013;368:1509–18. doi:10.1056/NEJMoa1215134
- Wang H, Xiong L, Tang W, Zhou Y, Li F. A systematic review of malignancy-associated hemophagocytic lymphohistiocytosis that needs more attention. Oncotarget. 2017;8(35):59977–59985. doi:10.18632/oncotarget.19230
- Behrens EM, Koretzky GA. Review: cytokine storm syndrome: looking toward the precision medicine era. Arthritis Rheumatol. 2017;69(6):1135-1143. doi:10.1002/art.40071
- Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ; HLH Across Speciality Collaboration, UK. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033-1034. doi:10.1016/S0140-6736(20)30628-0
- Weaver LK, Behrens EM. Weathering the storm: Improving therapeutic interventions for cytokine storm syndromes by targeting disease pathogenesis. Curr Treatm Opt Rheumatol. 2017;3(1):33–48. doi:10.1007/s40674-017-0059-x
- Treatment of COVID-19 patients with anti-interleukin drugs. ClinicalTrials.gov identifier: NCT04330638.
- SinoBiological (SB). Cytokine storm.
.png)
.png)







Comments
Post a Comment